Annals of Medical & Surgical Case Reports
Case Report
Immunotherapy Related Myositis: A Case Report
Litos I1*, Tsapakidis K1 and Tsoukalas N2
1Department of Medical Oncology, University of Thessaly, Larissa, Greece
2417 Veterans Hospital (NIMTS), Athens, Greece
*Corresponding author: Ioannis Litos, Department of Medical Oncology, University of Thessaly, Larissa, Greece, Tel: +302421074000; Email: johnli2784@gmail.com
Citation: Litos I, Tsapakidis K and Tsoukalas N (2019) Immunotherapy Related Myositis: A Case Report.Ann Med & Surg Case Rep: AMSCR-1000027.
Received date: 04 November, 2019; Accepted date: 09 November, 2019; Published date: 15 November, 2019
Abstract
Immune checkpoint inhibitors have revolutionized the treatment of many different types of cancers. These inhibitors work by blocking pathways called checkpoints. These checkpoint pathways are mechanisms for the human immune system to control the immune response. The immune checkpoint proteins cytotoxic T-lymphocyte–associated-4 (CTLA-4) and programmed cell death protein 1 (PD-1) are receptors expressed on the surface of cytotoxic T cells that interact ligands CD80/CD86 in the case of CTLA-4 andprogrammed death-ligand 1 (PD-L1) in the case of PD-1. Despite the often durable clinical benefits of the immune checkpoint blockade therapy, the use of immune checkpoint inhibitors is associated with a spectrum of adverse effects related to the mechanism of action that is quite different from other systemic therapies such as cytotoxic chemotherapy. The adverse effects can affect multiple organs of the body and are most commonly seen in the skin, GI tract, lungs and endocrine, thyroid, adrenal, pituitary, musculoskeletal, renal, nervous, hematologic, cardiovascular, and ocular systems, and there should be a high level of suspicion that any changes are treatment-related. This case refers to an immunotherapy induced myositis presented after ten cycles of nivolumab (anti PD-1 antibody).
Keywords: Immunotherapy; Musculoskeletal; Cardiovascular; T-lymphocyte
Case report
A 60-year-old man, who was a very heavy smoker (100 pack-years), was presented with cough, shortness of breath and hemoptysis and he finally was diagnosed with an adenocarcinoma of the lung stage IV (metastases of the bones).He received 6 cycles of Cisplatin and Pemetrexate without response and then he started immunotherapy with Nivolumab (total dose 240mg) every two weeks.
After having received ten cycles of Nivolumab, the patient was presented with a very elevated CPK (1800), but without any other symptom such as pain of the muscles. There were normal numbers of CK-MB, normal ultrasound of the heart, negative troponin test and negative check of immunology parameters.
An electromyography (Figure 1) was performed which was negative and a muscle biopsy revealed typical findings of myositis. He was administrated corticosteroids 1mg/kg daily for 1 week and progressively reduced them for a total duration of 4 weeks and finally he stopped immunotherapy. CPK levels became normal 3 weeks later and because Nivolumab therapy was considered a potential causative agent it was stopped. The patient is currently not on any active therapy and is undergoing active surveillance of his disease.
Discussion
The immune checkpoint proteins cytotoxic T-lymphocyte–associated-4 (CTLA-4) and programmed cell death protein 1 (PD-1) are receptors expressed on the surface of cytotoxic T cells that interact with their ligands CD80/CD86 in the case of CTLA-4 and programmed death-ligand 1 (PD-L1) in the case of PD-1. These pathways can be co-opted to help cancer cells to evade cytotoxic T-cell–mediated death [1].
Currently, there are several immune checkpoint inhibitors for the treatment of the cancer. Nivolumab targets PD-1 and has been approved for melanoma, metastatic non-small-cell lung cancer (NSCLC), head and neck squamous cancers, urothelial carcinoma, gastric adenocarcinoma, and mismatch-repair–deficient solid tumors as well as for classic Hodgkin lymphoma [2].
Despite the often durable clinical benefits of the immune checkpoint blockade therapy, the use of immune checkpoint inhibitors is associated with a spectrum of adverse effects related to the mechanism of action that is quite different from other systemic therapies such as cytotoxic chemotherapy. The adverse effects can affect multiple organs of the body and there should be a high level of suspicion that any changes are treatment-related. Immune checkpoint inhibitors therapy can usually continue in the presence of mild immune-related adverse events with close monitoring. However, moderate to severe adverse events may be associated with severe declines in organ function and quality of life, and fatal outcomes have been reported. These toxicities require early detection and proper management. Use of immune checkpoint inhibitors in patients with preexisting autoimmune disease or history of prior organ transplant requires an especially thoughtful discussion of potential risks and benefits [3-4].
Myositis is a disorder characterized by muscle inflammation with weakness and elevated muscle enzymes (CPK). Muscle pain can be present in severe cases and it can be life threatening if respiratory muscles or myocardium are involved. It can be found in 1.4% of the patients receiving immunotherapy and the therapy depends on the grade and on the severity of the symptoms [5-6].
If there is toxicity Grade 1 with mild weakness with or without pain of the muscles, you may continue immune checkpoint inhibitors, but, if there is CPK elevation, you may give oral corticosteroids and treat as toxicity Grade 2. If there is toxicity Grade 2 with moderate weakness with or without pain, you may temporarily withhold immunotherapy and resume upon symptom control or if CPK becomes normal, otherwise you may start corticosteroids 1mg/kg. If there is toxicity Grade 3-4 with severe weakness with or without pain, you should hold immune checkpoint inhibitors until toxicity Grade 1 or less and you should permanently discontinue if there is any evidence of myocardial involvement.
Conclusion
Although myositis is a rare clinical entity, it should be suspected in patients who receive immunotherapy. Clinicians should retain a high index of suspicion for immunotherapy related myositis and they should proceed to electromyography and biopsy of the muscles, because it is a side-effect irreversible, in most cases.
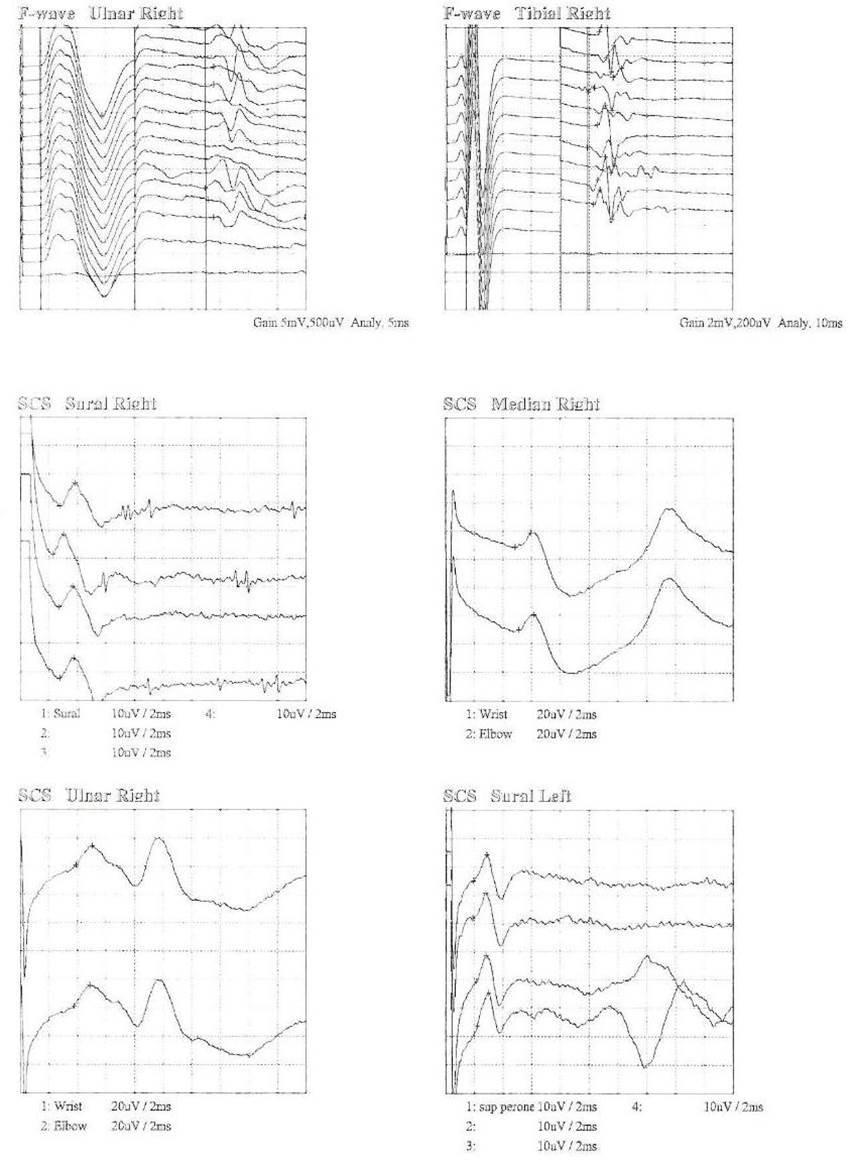
Figure1: Electromyography.
Citation: Litos I, Tsapakidis K and Tsoukalas N (2019) Immunotherapy Related Myositis: A Case Report.Ann Med & Surg Case Rep: AMSCR-1000027.