Annals of Medical & Surgical Case Reports
(ISSN 2652-4414)
Case Report
Incidental Finding of Silent Appendicitis on F-Fdg Pet/Ct in a 16-Year-Old Patient
EL BEZ Intidhar*Alsakran S, Tulbah R, Alghmlas F and Alharbi M
Department of nuclear medicine, King Fahad Medical City, Kingdom of Saudi Arabia, Saudi Arabia
*Corresponding author: EL BEZ Intidhar, Department of nuclear medicine, King Fahad Medical City, P.O. Box. 59046, Riyadh 11525, Kingdom of Saudi Arabia, Saudi Arabia,Tel: +966112889999 Ext: 21735; Email: elbez.intidhar@yahoo.fr
Citation: EL BEZ Intidhar, Alsakran S, Tulbah R, Alghmlas F and Alharbi M (2019) Incidental Finding of Silent Appendicitis On F-Fdg Pet/Ct in A 16-Year-Old Patient. Ann Med &Surg Case Rep: AMSCR-1000025.
Received date: 20 October, 2019;Accepted date: 03 November, 2019;Published date:12 November, 2019
Abstract
Acute appendicitis is a clinical diagnosis typically presenting with right lower quadrant pain. We describe the case of a 16-year-old man with case of T-cell acute lymphoblastic leukaemia (T-ALL) on chemo and chronic history disseminated mucormycosis infection on ambisome, who underwent Fluorine-18-Fluorodeoxyglucose Positron Emission Tomography (18F-FDG PET/CT). The scan showed incidental increased FDG uptake in the right base fossa likely related to the tip of the appendix. The ultrasound of the abdomen done the same day showed typical acute appendicitis symptoms. On further interrogation, the patient described a periumbilical pain for the past 7 day which was reliver by pain killers. Also, the patient had multiple episode of vomiting. The patient was treated medically by antibiotics, with good outcomes.
Keywords:Acute appendicitis; Increased FDG uptake in appendix; 18F-FDG PET/CT
Introduction
Acute appendicitis is caused by luminal obstruction commonly due to fecalith which then progress to luminal distention and inflammation [1]. Acute appendicitis is diagnosed passed primarily by imaging while clinical manifestations and laboratory tests assume supportive role [2]. The described sonographic findings for appendicitis include blind ended tubular structure with thickened wall and increase caliber of more than 6 mm [3,4]. The CT scan appearance of acute appendicitis are increase appendiceal caliber, periappendiceal inflammation (fat stranding, thickening of the lateral conal fascia), free fluid, enlarged lymph nodes and appendicolith[3,4].
Positron emission tomography (PET) is being utilized for diagnosis and staging of different malignancies for example lymphoma, pulmonary nodules, and colorectal cancers [5-7]. The PET scan shows the abnormal metabolic activity at the molecular level even if no abnormal morphology is demonstrated in anatomical imaging [8]. F-18 fluorodeoxyglucose (FDG) is the most commonly used tracer for PET imaging [9]. The FDG acts like glucose and thus accumulate is in a giving tissue proportional to glycolysis. Malignant cells have increased glucose metabolism (glycolysis) and appear hot on PET scan [9].However, FDG is not malignancy specific, it can accumulate in many benign causes, most commonly inflammation [10]. There are only few reported cases of acute appendicitis detected using 18 F-FDG PET/CT in the literature [11].
We describe a case of an asymptomatic 16-year-old man, who underwent 18F-FDG PET/CT, with incidental increased FDG uptake in a tubular structure adjacent to the cecum, suggesting acute appendicitis.
Case report
The patient is a 16 years old male known case of T-cell acute lymphoblastic leukaemia (T-ALL) on chemo. He has chronic history disseminated mucormycosis infection complicated nephric abscess and lung infection. Their involve were refractory to medical treatment, so he underwent right nephrectomy and right upper lobectomy one year ago.Now the patient underwent 18 F-FDG PEC/CT for assessing the treatment response to ambisome to control his infection. 18 The PET/CT scan was obtained 60 minutes after the injection of 200 MBq of F-uorodeoxyglucose.
The scan showed intense focus of FDG uptake at the right base fossa likely related to the tip of the appendix (maximum standardized uptake value SUV max 4.5), associated with minimal surrounding fat stranding (Figure 1). The patient was asymptomatic at the time of imaging. 18F-FDG PET/CT findings were highly suspicious for acute appendicitis even in this patient was asymptomatic. At the time of interpretation, the ordering provider was contacted and informed of the findings. The patient was then sent to the emergency department where he underwent abdominal US, on the same day. The US showed 0.8 cm appendix as a tubular blinded structure in the right iliac fossa with surrounded small amount of free fluid (Figure 2).
On further interrogation, the patient described a periumbilical pain for the past 7 day which was reliver by pain killers. Also, the patient had multiple episode of vomiting. The patient was treated medically by antibiotics, with good outcomes.
Discussion
The lifetime risk of acute appendicitis is between 6% and 9% [12]. Its incidence was calculated at 86 per 100,000 per year [13]. Therefore, only few observations of appendicitis diagnosed on 18F-FDG PET/CT have been reported [14-19]. In 4 reports, symptomatic patients underwent 18F-FDG PET/CT in the work-up of a palpable right abdominal lower quadrant mass. In each of these patients, 18F-FDG uptake in the mass was noted, with SUVmax values varying from 7.27 to 22. At surgery, each of these masses was shown to be a plastron appendicitis, in which the inammation of the appendicial wall spreads into the surrounding mesenteric fat [14-16]. In other report [17], an 18F-FDG avid appendicitis (SUV 6.9) was shown to be secondary to invasion by a small cell lung carcinoma, a rare cause of appendicitis based on obstruction of the appendicial lumen resulting in inammation and possibly even perforation. These patients may remain asymptomatic until the lumen of the appendix is totally occluded [17, 22, 24]. Two more patients showed 18F-FDG uptake in appendicitis, which was almost asymptomatic. In one, appendicitis was revealed by 18 PET/CT during post therapy [20-23] assessment of a metastatic germ cell carcinoma (SUV 6.9) [18] and the other was revealed on restaging of a squamous head and neck carcinoma (SUV 4.3) [19]. In the latter patient, the pathology revealed subacute upon chronic appendicitis. In the current case report, our patient was also asymptomatic at the time of the scan. The nuclear physician and clinician should be aware of this possibility.
The paucity of clinical findings in our patient may relate to the absence of peri-appendicular inflammation. Some cases of asymptomatic appendicitis had already been documented in a few reports [25-29]. One instance of appendicitis without abdominal pain was described in an asymptomatic neutropenic patient [27]. Likewise, absence of leukocytosis was absorbed in asymptomatic patients who had been given platinum-based chemotherapy for extraintestinal neoplasia and were probably neutropenic [17,18]. Anyhow, given the many millions of 18F-FDG-PET/CT scans that are performed yearly, asymptomatic acute appendicitis [17,18] seems to be a rare occurrence.
While 18F-FDG PET-CT should not be used for evaluation of suspected acute appendicitis, 18F-FDG PET-CT may occasionally suggest the diagnosis when it is an incidental finding or is unsuspected, such as in patients with a fever of unknown origin. On FDG PET-CT, acute appendicitis presents as focal hypermetabolic activity overlying an enlarged and dilated appendix with periappendiceal fat stranding [30]. Typhlitis, a life-threating necrotizing enterocolitis involving the ileocecal region predominantly seen in neutropenic patients, may demonstrate similar increased FDG avidity in the region of the appendix with involvement of the adjacent bowel [30].
The patient described in our report was treated medically. Although to our knowledge no cases have been published so far in which antibiotics were the only treatment used, PET could be used as a way to monitor disease activity [29].
Conclusion
18F-FDG PET-CT is commonly used in the evaluation of neoplastic processes; however, FDG avidity is not tumor-specific, as a myriad of infectious and inflammatory processes may show increased metabolic tracer activity as well. The appendicitis, just like all inflammatory processes, may cause increased 18F-FDG uptake. Therefore, even with the asymptomatic patient, the clinician should be aware of the possibility of silent appendicitis. This case of acute appendicitis illustrates that the interpreter of 18F-PET-CT images must consider that FDG activity may reflect pathology unrelated to the primary indication for the exam.
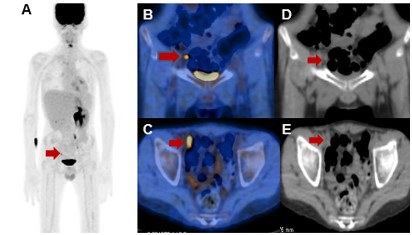
Figure 1: 18F-FDG PET/CT scans showing intense focus of FDG uptake at the right base fossa (red arrow) likely related to the tip of the appendix (SUV max 4.5), associated with minimal surrounding fat stranding: A, maximum intensity projection PET; B, coronal fused PET/CT image, C, axial fused PET/CT image, D, coronal CT image, E, axial CT images.
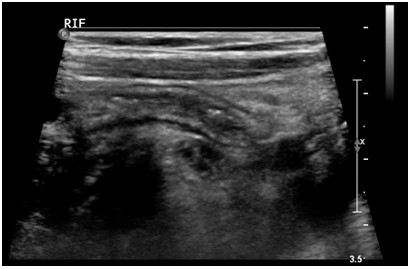
Figure 2: There is tubular blind ended structure (appendix), which measures 0.8 cm.
Citation: EL BEZ Intidhar, Alsakran S, Tulbah R, Alghmlas F and Alharbi M (2019) Incidental Finding of Silent Appendicitis On F-Fdg Pet/Ct in A 16-Year-Old Patient. Ann Med &Surg Case Rep: AMSCR-1000025.