Clinical Orthopedics Advanced Research Journal
Case Report
Trans-Scaphoid Perilunate Dislocation with Fractured Triquetral Bone in A Pediatric Patient: A 10-Month Follow Up of a Case Report
Teodonno F*, Macera A, Crespo Lastras P, Cervero Suárez FJ, Suárez Rueda C and Márquez Ámbite J
Department of Orthopedic Surgery and Traumatology, Infanta Elena Hospital, Valdemoro, Madrid, Spain
*Corresponding author: Francesca Teodonno, Department of Orthopedic Surgery and Traumatology, Infanta Elena Hospital, Valdemoro, Madrid, Spain, Tel: +34918948410; Email: fra.teodonno@hotmail.com
Citation: Francesca Teodonno, et al. (2019) Trans-Scaphoid Perilunate Dislocation with Fractured Triquetral Bone in A Pediatric Patient: A 10-Month Follow Up of a Case Report. Clin Ortho Adv Res J: COARJ-100003.
Received date: 28 October, 2019; Accepted date: 04 November, 2019; Published date: 15 November, 2019
Abstract
Transcarpal fractures and dislocations in pediatric patients are seldomly reported in literature. Trans-scaphoid dislocations represent only the 1.4% of all scaphoid fractures in the pediatric population. We present the case of 12-year-old boy that, after a fall on the outstretched hand from a motorbike, sustains a trans-scaphoid perilunate dislocation with non displaced fractures of the scaphoid and triquetrum bones, and was treated conservatively through closed reduction for the dislocation and immobilization with a closed cast. At final follow up of 10 months, the fractures healed well with a full return of good wrist function. This unusual injury is described so that it may be better acknowledged in the future.
Keywords: Fractures healed; Orthopedic Surgery; Triquetral Bone; Trans-Scaphoid Perilunar Dislocations;
Introduction
Trans-scaphoid perilunate dislocations are extremely uncommon among pediatric patients, but may not be as rare as their small presence in the literature suggests [1,2]. A retrospective analysis published by [3] suggests that these lesions represent only the 1.4% of all scaphoid fractures in the pediatric populationThe carpus of the child is entirely cartilaginous and the vulnerability of the radius to fracture makes it relatively immune to injury. As the ossification of the carpus begins, its injury patterns become more similar to those of adults. Lunate and perilunate dislocations usually occur from high energy mechanisms [3,4]. We present the case of a trans-scaphoid perilunate dislocation with fractured triquetral bone in a pediatric patient. To the best of our knowledge, a case of this type has not been reported in pediatric patients previously.
Case Report
We present the case of a 12-year-old boy that arrives at the Emergency Room (ER) after having fallen at high speed from a motorbike onto his out streched dominant hand. An initial evaluation showed a silver-fork deformity of the right wrist, important swelling, no haematoma, pain with the palpation of the distal radioulnar joint as well as the proximal carpal row. The patient was unable to move his right wrist without pain. No median nerve nor other nerve injury as well as vascular injury was observed. Radiography of the hand and wrist showed a fracture of the scaphoid in the anteroposterior (AP) view and a dorsaltrans-scaphoid perilunate dislocation in the lateral (L) view (Figure 1). The patient was sedated in the ER with nitrous oxide (Kalinox), Air Liquide Santé International, France) and a closed reduction was accomplished by applying a constant traction of the hand for ten minutes and hyperextending the wrist while maintaining the traction and pressing with the thumb against the lunate towards the dorsal side; then the hand was forced into flexion. The wrist was immobilized with a closed cast including the proximal phalanx of the thumb and with the wrist in slight flexion (Figure 2).
A radiography and a CT scan post-reduction were performed, validating a correct alignment of the carpal bones. The CT clarified the fracture pattern (Figure 3,4), showing an undisplaced fracture of the waist of the scaphoid and a marginal fracture of the radial proximal pole of the triquetral. We decided to follow a conservative treatment due to the results of the CT scan. Radiographical and clinical controls were performed after 5 days and 2 weeks verifying no secondary displacement of the fractures. After a radiographic control, the cast was removed after 6 weeks; no pain with the palpation of the scaphoid was observed. The patient had a complete passive movement of the wrist and an active ROM of 50º of dorsal flexion and 80º of palmar flexion. A diminished strength compared to the contralateral side was observed with the fist grip and pincer grip.
After 8 weeks the patient started the rehabilitation program, and after 2 weeks the patient gained 20º of active movement, reaching a wrist ROM of 70º of dorsal flexion and 80º of palmar flexion.
The fist grip and pincer grip strength was equal to the contralateral side. Passive movement was symmetrical with the contralateral wrist. No pain was observed. The radiography of the 12-week’s review (Figure 5) showed an augmented scapholunate space of 4.46 mm (Terry Thomas sign) and a dorsal intercalated segment instability (DISI) of the scaphoid, with a scapholunate angle of 71º and a radiolunate angle of 29º. These findings were not detected in the previous radiographies. The patient presented complete mobility and no pain so we opted for a wait and see treatment.
These findings were ulteriorly studied by performing an MRI of the hand and wrist (Figure 6) that was realized 7months after the injury, showing edema of both fragments of the scaphoid bone and in the triquetral bone, delayed union of the scaphoid fracture and integrity of the scapholunate ligaments, although DISI deformity was observed. The physical examining showed no pain in the scaphoid bone, conserved ROM compared to contralateral hand, minus for a-8° limitation for dorsal flexion and preserved strength in comparison to the other hand. Physiotherapy was prescribed, as well as swimming.
At the final follow up of 10 months (Figure 7,8) radiography showed signs of consolidation of the scaphoid bone, scapholunate space of 3.47 mm, scapholunate angle of 68° and a radiolunate angle of 22°. Compared to the previous follow up, the patient presented a better ROM, with a -5° limitation of dorsal flexion compared to the contralateral hand. Watson test was negative. The patient was dismissed and fully returned to sports.
Discussion
Carpal injuries are uncommon in the pediatric population, although studies suggest that the incidence is increasing [5]. With changes in patient characteristics and activities, these injuries in children and adolescents are now matching the published patterns in adults [3].
Perilunate dislocations normally occur from high energy mechanisms such as motor vehicle and sports accidents. The mechanism of injury is often a hyperextension of the wrist during a fall on the outstretched hand along with the ulnar deviation and carpal supination [6]. The more intense participation in competitive youth sports may be the cause for the increased occurrence of these injuries in the pediatric population [7].
The pathomechanics of perilunate dislocations were studied by [4], who classified carpal dislocations in four stages, each one representing a sequential intercarpal injury, beginning with the scapholunate joint disruption, followed by sequential ligamentous disruption in the radial to the ulnar direction. A scapholunate dislocation is classified as a stage 1 injury; a stage 2 injury involves dislocation of the lunocapitate joint. The disruption of the lunotriquetral joint produces a stage 3 injury and lunate dislocation with volar rotation is considered as a stage 4 injury. This can be associated with osseous injury of the greater arc of the wrist causing fracture-dislocations [8].
As for the presence in literature of similar injuries, [1] reported a case of a 10-year-old patient with a dorsal trans-scaphoid perilunate dislocation treated with a closed reduction and immobilization with a dorsal brachial plaster slab, including the proximal phalanx of the thumb, and with the wrist in slight flexion. The slab was removed seven weeks later and full non painful range of motion was reached at nine weeks. No triquetral bone fracture was described in this case. Also Ji et al [2] recorded a case of a 10-year-old boy that after a traumatism presented fractures of the scaphoid, capitate and triquetrum associated to a dorsal trans-scaphoid perilunate dislocation. A closed reduction was performed and further stabilization was achieved by multiple Kirschner wires across the reduced fractures. The capitate was augmented with autogenous bone graft from the distal radius. The wrist was immobilized with a cast for 12 weeks. At 1 year post-surgery, ROM was 70º-0º-80º. Grip strength was approximately 85% of the contralateral side. Radiographs and 3D-CT scans taken 6 years after the surgery showed well healing of the fractures and no evidence of any growth abnormality or arthritic changes.
The treatment of scaphoid fractures in pediatric and adolescent patients is dependent on location of the fracture and displacement. The cast immobilization of acute, nondisplaced fractures results in a union rate of >90% [9]. As for the treatment of perilunate dislocations, the general recommendation is surgery, due to the extensive ligamentous injuries and inherent carpal instability [7-10]. It is considered that it leads to better functional outcomes when compared with nonoperative treatment. Nevertheless patients can experience loss of grip strength, chronic wrist pain, loss of motion and radiographic signs of arthritis and carpal collapse despite optimal management. Also, clinical outcomes are often significantly better than radiographic outcomes. Compliant to the nonoperative treatment of these injuries, the closed reduction is difficult to achieve [11], although it is more likely to succeed in perilunate than with lunate dislocations owing to the greater extent of ligamentous disruption with the latter, and also if the time duration between the injury and the closed reduction is the shortest possible [7]. Reports in literature suggest also that ligament injuries of the immature wrist are less common than osseous due to the viscoelastic properties of the carpal structure [2,8]. If no residual instability is witnessed after a closed reduction, conservative treatment is a possibility in pediatric patients. In our case we opted for it, as our patient presented stability after the reduction and open physes. Furthermore, the wrist was immobilized for 8 weeks, following Peiróa’s experience1, as a difference with other authors that prefer an immobilization of 12 week [2]. These lesions in adults require generally a 3-month immobilization [10].
Unfortunately, limited information was found in literature concerning long term complications such as arthrosis and wrist instability, due to the rarity of these injuries. As of the late union of the scaphoid, [5] found that isolated acute waist fractures treated conservatively healed successfully, with no incidence of delayed or nonunion [3] described a 22% of union in acute displaced waist fractures and 92% of union in acute non displaced ones. In general, nonunion is an important complication of perilunate dislocations that usually leads to surgery [3,9,10]. Our patient had an asymptomatic delayed union, so we considered that an enhanced physiotherapy program was a possible treatment before opting for surgical solutions, due also to the age of the patient.
The presence of a scapholunate space of 3.47 mm at the final follow-up was not relevant in our opinion considering the article published by [12] studied the normal values for age in pediatric population of the scapholunate interval. For a 12-year old boy, is it estimated as normal values until 4.5 mm. The scapholunate interval is normally wider compared to adults due to the large chondral component to the carpus. Our patient presented also a scapholunate angle of 68º and a radiolunate angle of 22º, that in adults are considered signs of carpal instability, but again in the pediatric population the relationship between the measurements and the clinical significance are not clear. Some authors consider that with the carpus completely ossified the applicability of standard adult carpal angle values is valid [13] and other authors that radiographically markers of carpal instability should be considered against age-matches values, and are to be associated in adolescents and pediatric patients with a pathological physical exploration, such as local discomfort [14]. Considering that our patient was asymptomatic at the final follow-up, no ulterior tests were performed.
Conclusion
The increase of incidence of carpal fractures and dislocations in pediatric patients creates a challenging problem, treatment related. This unusual injury is described so that it may be better acknowledged in the future. Also, surgeons should attempt to obtain long-term follow-up on the patients to document the efficacy of the procedures in order to assess better the treatments available and the prospective of osteoarthritis.

Figure 1: Trans-scaphoid perilunate dislocation.
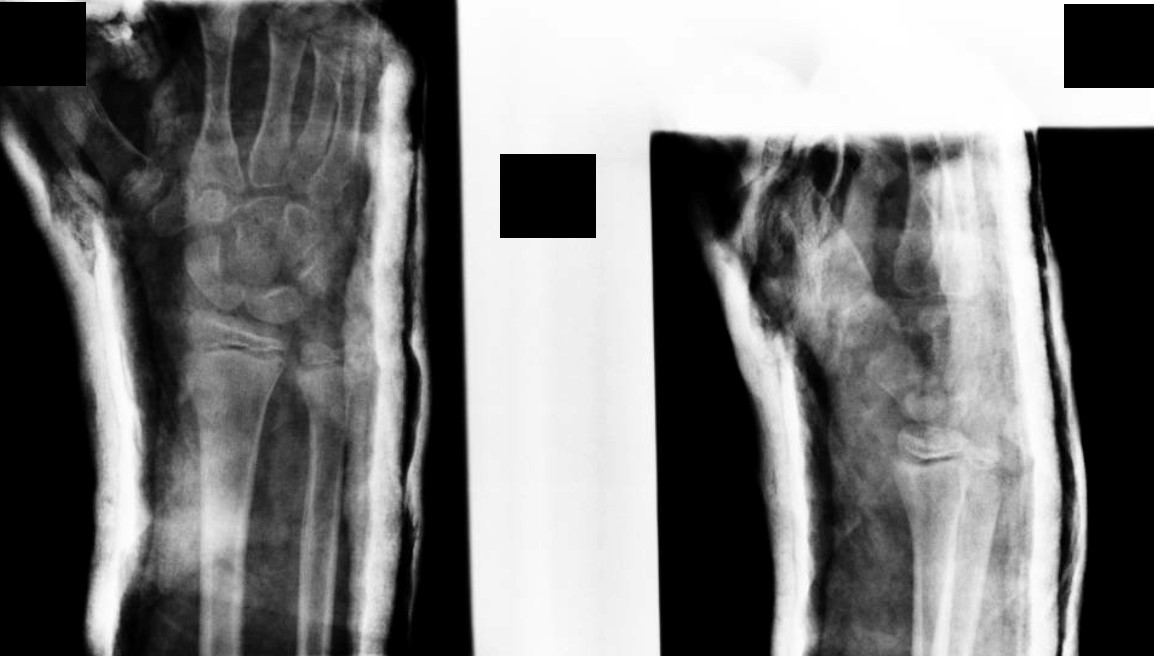
Figure 2: Post-reduction aspect.

Figure 3: Post-reduction CT scan. Coronal view.
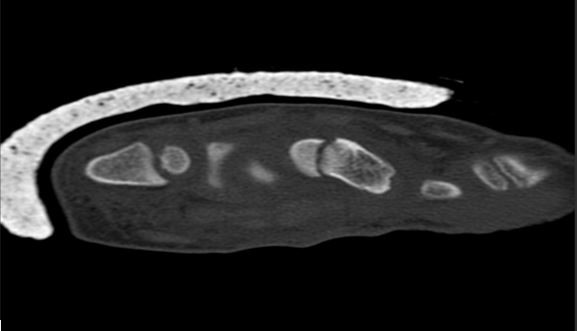
Figure 4: Post-reduction CT scan. Sagittal view of the scaphoid fracture.
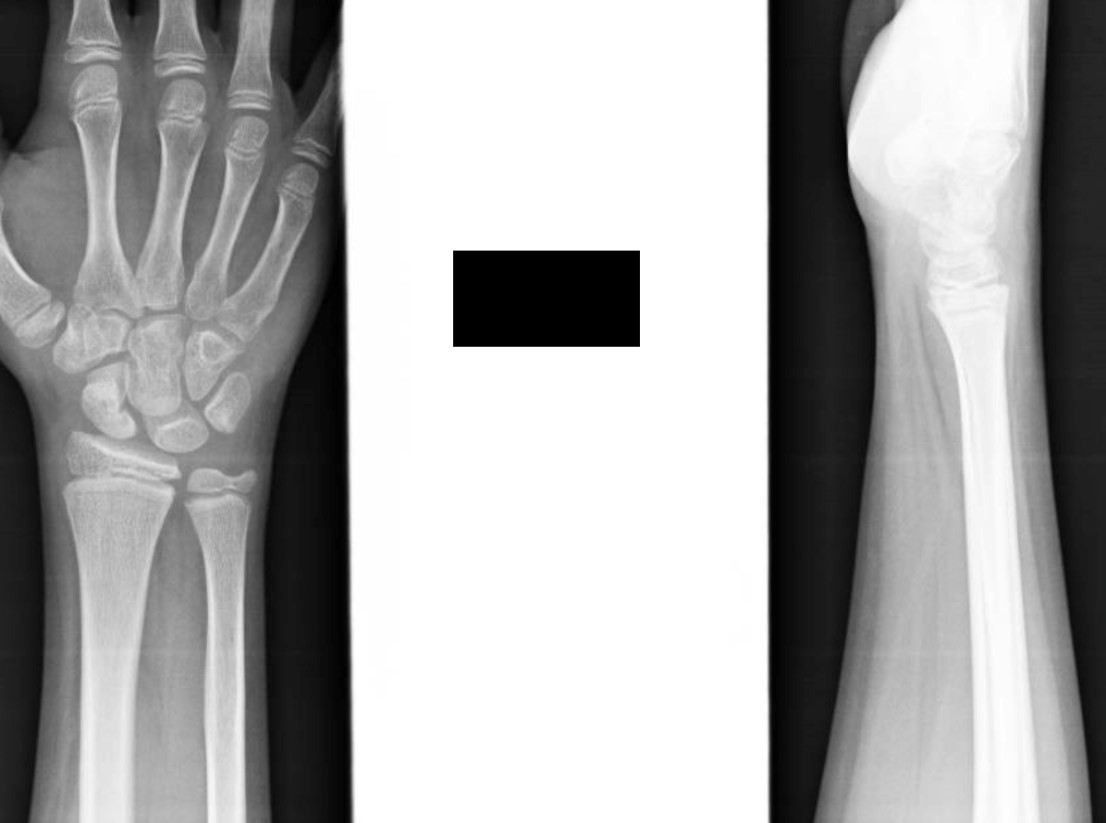
Figure 5: 12 weeks: Positive Terry Thomas’s sign and DISI deformity.

Figure 6: MRI view.
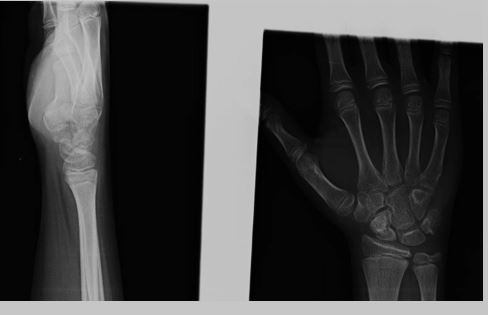
Figure 7: Radiographical aspect of the final follow-up.

Figure 8: Final follow-up.
Citation: Francesca Teodonno, et al. (2019) Trans-Scaphoid Perilunate Dislocation with Fractured Triquetral Bone in A Pediatric Patient: A 10-Month Follow Up of a Case Report. Clin Ortho Adv Res J: COARJ-100003.