Emergency Medicine and Trauma Care Journal
Case Report
Direct Current Cardioversion Terminating a Supraventricular Tachycardia with High Lateral Pre-Excitation Rather than Hypertension Normalization; A rare presentation; A case report
Elsayed YMH1*
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
*Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt, Tel: +20156645606; Email: dryaser24@yahoo.com
Citation: Elsayed YMH (2019) Direct Current Cardioversion Terminating a Supraventricular Tachycardia with High Lateral Pre-Excitation Rather than Hypertension Normalization; A rare presentation; A case report. Emerg Med Trauma Care J: EMTCJ-1000014.
Received date: October 18, 2019; Accepted date: 22 October, 2019; Published date: 30 October, 2019
Abstract
Rationale: Regular wide-QRS complex tachycardia is one of the most critical serious arrhythmia. Correct diagnosis for wide complex tachycardia remains a challenge. This is despite the presence of numerous differentiating criteria between ventricular tachycardia and supraventricular tachycardia. Stress and alcohol is a well-known arrhythmogenic substance. Unstable arrhythmia is the immediate indication for using direct current cardioversion.
Patient concerns: A 50-year-old heavy-smoker, alcoholic, male patient presented with unstable regular wide-QRS complex tachycardia had happened post-stress.
Diagnosis: Unstable regular wide QRS-complex tachycardia with hypertension was the initial diagnosis. Suggested supraventricular tachycardia with high lateral pre-excitation in state of anxiety-related sympathetic excessive activity was the final diagnosis.
Interventions: Oxygenation, Valsalva maneuver trial, sedation, ECG monitoring, and direct current cardioversion shock.
Outcomes: Dramatic terminating of unstable wide QRS-complex tachycardia with normalization of hypertension.
Lessons: Supraventricular tachycardia with high lateral pre-excitation is a new presentation. Alcohol may be inducing a serious arrhythmia and unstable regular wide-QRS complex tachycardia, especially in heavy cigarette-smoker. Normalization of hypertension post-direct current cardioversion shock.
Keywords: Direct current cardioversion; high lateral pre-excitation; hypertension; Supraventricular tachycardia; Wide QRS-complex tachycardia
Abbreviations
AV : Atrioventricular
BBB : bundle branch block
DCC : Direct current cardioversion
DD : Differential diagnosis
ECG : Electrocardiogram
ICU : Intensive care unit
LAD : Left axis deviation
PVCs : Premature ventricular contractions
SVT : Supraventricular tachycardia
VR : Ventricular rate
VT : Ventricular tachycardia
WPW : Wolff-Parkinson-White syndrome.
Introduction
A correct diagnosis of broad QRS-complex tachycardia is still a challenge [1]. Wide QRS-complex tachycardia is known as a heart rate of more than 100 bpm and QRS duration of more than 120 ms [1]. Since 1978, various electrocardiographic (ECG) criteria have been proposed for the differential diagnosis of wide-complex tachycardias, especially with the existence of atrioventricular (AV) dissociation, and the axis, duration and morphology of QRS-complexes [1]. Although there are wide helping criteria, diagnosis of wide-complex tachycardias is still so difficult. Thus, errors can have serious consequences. To reduce such errors, several differential diagnosis (DD) algorithms have been proposed since 1991 [1]. However, there is a small percentage of wide QRS tachycardias the diagnosis is still uncertain1. The following three issues are the main DD for a wide QRS complex tachycardia:
Data from clinical history and physical examination may help identify the origin of the arrhythmia [1]. VT is the most common cause of wide QRS tachycardia (80%) [3]. It is strongly suggested by a history of structural heart disease like-myocardial infarction or congestive heart failure [4] A history of like attacks suggests SVT [5]. Physical findings that suggest AV dissociation, such as cannon A-waves in the jugular venous pulse, variable intensity of S1, or variable blood pressure unrelated to breathing, point towards a ventricular origin [6]. On the other hand, if the tachycardia can be terminated by maneuvers such as the Valsalva maneuver, this strongly suggests a supraventricular origin [1]. Another important aspect of physical examination is hemodynamic stability, which is crucial for treatment in the acute phase [1]. Correct diagnosis in wide-complex tachycardia remains a challenge despite the many criteria for differentiating between VT and SVT [1]. The standard 12-lead ECG is the most important diagnostic method for describing the origin of tachyarrhythmias [1]. Since 1978, various electrocardiographic criteria have been proposed for the differential diagnosis of wide complex tachycardias, most of them depend on the existence of AV dissociation and the axis, duration and morphology of QRS-complexes [1].
Wolff-Parkinson-Whie (W) syndrome is a disorder characterized by presence of an accessory pathway which predisposes patients to tachyarrhythmias and sudden death [7]. Historically, Wolff, Parkinson, and White first identified the syndrome in193 in a series of 11 healthy young adults with a functional BBB, an abnormally short PR-interval and paroxysms of SVT [6]. The diagnosis of WPW syndrome is reserved for patients who have both pre-excitation and tachyarrhythmias [7]. Wolff-Parkinson-White syndrome is not uncommon in the cardiac emergency [8]. Delta waves detectable on an ECG have been reported to be present in 0.15% to 0.25% of the general population7. The anomaly in WPW syndrome is accessory connections between the atrium and ventricle. This accessory connection which is called Bypass tract may be atriofascicular, fasciculoventricular, intranodal, or nodoventricular, the most common being atrioventricular (AV) pathway otherwise known as a Kent bundle. Conduction through a Kent bundle can be anterograde, retrograde, or both [7]. Most patients with the WPW syndrome have Otherwise normal hearts, but some have concomitant congenital heart disease [7]. The main ECG features of pre-excitation are a short PR-interval (<0.12 seconds), a prolonged QRS complex (>0.12 seconds), and a slurred, slow rising onset of the QRS-complex that is known as the delta wave [7]. Immediate cardiac referral is important for risk stratification via electrophysiological study [8]. Patients with wide complex tachycardias that associated with a bypass tract like-WPW have a short refractory period with a risk for rapid rates and ventricular fibrillation. Thus, adenosine, B-blockers, and calcium channel antagonists are contraindicated. Procainamide is the drug of choice for WPW syndrome with wide complex tachycardia [9].
Case presentation
A 50-year-old married male, heavy-smoker, Egyptian glass-seller presented to the emergency department with palpitations, dizziness, and presyncope. Symptoms had happened after anxiety event. The patient gave history of the same attack 3-years ago. The patient declared the presence of old history of substance abuse like hashish, marijuana, alcohol, and heroin. The patient is still alcoholic drinker. The patient denied any history of other cardiac, thyroid, or other relevant diseases. Upon examination, the patient appeared irritable, sweating profusely, tachypnic, and anxious. His vital signs were as follows: blood pressure of 150/100 mmHg, the pulse rate of 220/bpm; and regular, the respiratory rate of 26/min, the temperature of 36.8°C, the pulse oximeter of O2 saturation of 94% and tachycardia on heart auscultation. No more relevant clinical data were noted during the clinical examination. The initial workup was: electrocardiogram (ECG), that showed regular wide QRS-complex tachycardia at 210 beats/min with left axis deviation (Figure 1,2 A-B) The patient was admitted to ICU and managed as unstable wide QRS-complex tachycardia. Oxygen inhalation (5 L/min) was given. Intravenous midazolam (2.5 mg over 5 minutes) was urgently given aiming for direct current cardioversion (DCC) shock procedural preparation. One spontaneous synchronized monophasic DCC shock (200 J) was given. The ECG recordings post-DCC shock showed abrupt disappearance of tachycardia. The patient was already connected to the ICU monitor for vitals and O2 saturation follow up. ECG tracing was repeated after the DCC shock (Figure 2 C-D). The investigations done were troponin test, electrolyte levels, complete blood count, thyroid studies, and random blood sugar with no detectable abnormal results. Echocardiography showed anterior and inferior hypokinesia with EF 51%. Complete recovery achieved and the patient was discharged within 6 hours from admission with no any problem. Amiodarone (oral tablet) 200 mg once daily on morning was prescribed on discharge. Planning for future electrophysiological study was recommended.
B. tracing upon arrival to ICU department with halve calibration showing the same changes of A. tracing.
C. tracing after DCC shock showing sinus tachycardia, ST-segment depressions in I, aVL, V5, and V6 leads (blue arrows), PVCs in V1-3 leads (lemon arrows), delta-wave in I, and aVL leads (orange arrows), T-wave inversions in inferior leads (II, III, and aVF) (purple arrows), with ventricular rate of 88 bpm. D. tracing after 60 minute post-DCC shock showing the same changes of C. tracing with disappearance of PVCs.
Discussion
Overview: A 50-year-old male, heavy-smoker, and alcoholic patient presented with unstable regular wide QRS-complex tachycardia and hypertension post-emotional stress.Ventricular tachycardia was excluded after using the following algorithms that are helping in differentiation of wide QRS-complex tachycardia.
Four-stepwise Morphological criteria of Brugada algorithm
Morphological criteria for VT present in both leads V1 and V6.
Vereckei algorithm
• Supraventricular tachycardia with BBB was not coincided with ECG.
• Supraventricular tachycardia with AV conduction via an accessory pathway become the most suggested final diagnosis.
• The pre-excitation appeared in the high lateral leads (I, and aVL) is a new pre-excitation affection for further electrophysiological study.
• I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison.
• Study question here: How did the DCC terminating the unstable regular wide QRS-complex tachycardia and normalizing the elevated blood pressure?
• The primary objective: For my case study was the presence of unstable regular wide QRS-complex tachycardia with hypertension after emotional stress in a smoker and alcoholic patient.
• The secondary objective: For my case study was the dramatic termination of unstable wide QRS-complex tachycardia and normalizing the elevated blood pressure with a single DCC shock (200J).
• Limitations of the study: There are no known limitations for the study.
• Recommendations: It is recommended to widening the research in clearing the effect of DCC shock on hypertension. It is advised to focus an electrophysiological study research on the high lateral pre-excitation.
Conclusion
Dramatic termination of unstable regular wide QRS-complex tachycardia and normalizing the elevated blood pressure with DCC shock. Presence of a new high lateral pre-excitation with supraventricular tachycardia.
Acknowledgement
I wish to thank critical care unit nurses who make extra ECG copies for helping me.
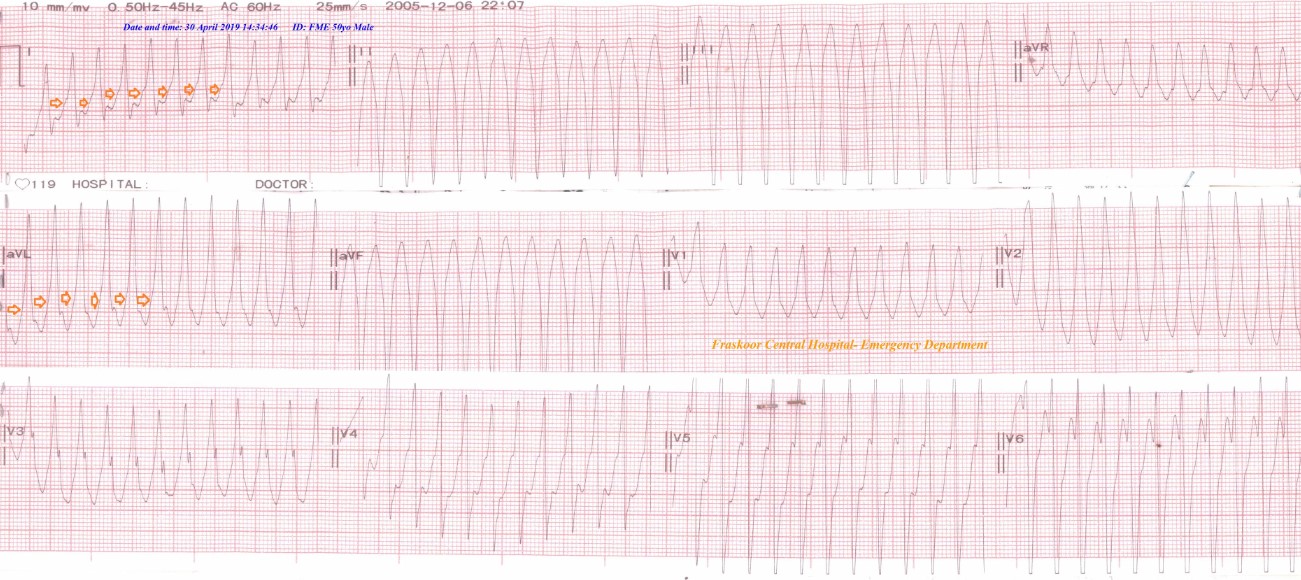
Figure 1: ECG tracing upon arrival in the emergency department showing regular wide QRS-complex tachycardia, delta-wave in I, and aVL leads (orange arrows) with ventricular rate (VR) of 210 bpm with marked LAD (-78°C).
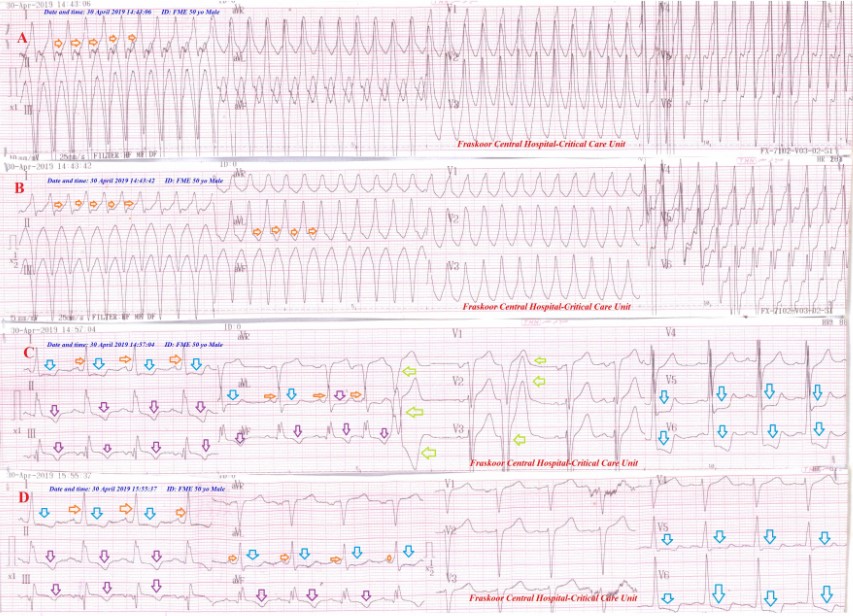
Figure 2: ECG tracings A. tracing upon arrival to ICU department showing regular wide QRS-complex tachycardia delta-wave in I, and aVL leads (orange arrows), with VR of 200 bpm with marked LAD (-78°).
Citation: Elsayed YMH (2019) Direct Current Cardioversion Terminating a Supraventricular Tachycardia with High Lateral Pre-Excitation Rather than Hypertension Normalization; A rare presentation; A case report. Emerg Med Trauma Care J: EMTCJ-1000014.