Annals of Pediatrics and Child Care
Case Report
Chylothorax Complicating Difficult Removal of Port-A-Cath in A Child with Acute Leukemia
Nazir H*
Faculty of Medicine, Alexandria University, Egypt
*Corresponding author: Hanan Nazir, Faculty of Medicine, Alexandria University, Egypt, Tel: + +96896556198, Email: dr.hanannazir@yahoo.com
Citation: Hanan Nazir (2019) Chylothorax Complicating Difficult Removal of Port-A-Cath in a Child with Acute Leukemia. Ann Pediatr Child Care: APCC-100010.
Received date: 22 October, 2019; Accepted date: 29 October, 2019; Published date: 5 November, 2019
Abstract
Portacath devices are widely used among young children with leukemia to secure a central venous line for administration of chemotherapy, blood products and antibiotics. The completely embedded device is usually inserted at the start of chemotherapeutic protocol, and stays in situ for around 6 months after completion of the full course. Complications during removal of portacath are relatively rare. Retention of segments of portacath in the central veins have been reported in 2.2%. We report on a rare incidence of development of chylothorax on an attempt to remove a stuck portacath. The patient was managed conservatively with good outcome.
Keywords: Acute leukemia; Chylothorax; Port-A-Cath
Case summary
MN is a 4 year- old girl with pre B-ALL, who completed treatment according to UKALL protocol in August 2015. Seven months’ post chemotherapy, she was electively admitted to hospital for removal of her Port-A-cath. The Port-A-cath was embedded in the vessel wall, and attempt to remove it failed, ending in removal of the device and the distal tunneled part with retention of proximal end of the catheter. Post operatively the patient developed progressively worsening swelling over the left side of the neck, that later extended down to the supraclavicular region and over the anterior chest wall (Figure 1).
Next day, chest x-ray showed left sided pleural collection (blue arrow) (Figure 2). CT chest confirmed the position of the retained part of the central catheter (black arrow) along the brachiocephalic vein, ending at the confluence of SVC and right atrium. She was electively intubated in the PICU and a pigtail catheter (Figure 3) was inserted under US guidance, which initially drained 288 ml of milky fluid. Analysis of the pleural fluids revealed Cholesterol level of 1.2 g/L, Triglycerides of 4.8 g/L and HDL of 0.22 g/L, confirming the diagnosis of chylothorax. She received prophylactic antibiotics and nutritional support in the form TPN for 7 days followed by fat free diet for 6 weeks. Later, she resumed normal diet with no clinical or radiological worsening. On follow up, the patient remained stable and the retained part of portAcath device remained in place for almost 3 years with no symptoms, evidence of thrombus, infection, or catheter migration.
Discussion
Totally implanted central venous catheter are widely used in children with hematologicmalignancies to establish a reliable venous access. Young infants, with their tiny veins, and other children whose treatment protocols imply more intensive chemotherapy are expectedly candidates for those lines. Central line related- blood stream infection and malfunction with obstruction/ thrombosis of venous catheter are among the most frequently encountered complications associated with Port-A Cath use in clinical practice. On the other hand, some rare complications are sometimes seen.
In the current case, attempt to remove Port-Acath was complicated by the development of chylothorax, a complication that was not reported earlier. Postoperative chylothorax results from injury to the thoracic duct, and is commonly reported following mediastinal, lung, heart, and esophageal surgery [1,2]. The anatomical unpredictability of the thoracic duct renders it susceptible to injury, even in the hand of an experienced surgeon.
It was postulated that fixation of the retained parts of central venous catheters results from formation of fibrin sheath around the indwelling catheter, and sometimes vein wall thickening along the length of the catheter. The catheter becomes fixed to the vessel wall through bridging between the vein wall and neo-endothelium of the fibrin sheath +/- calcification. Such fixation made it difficult for the catheter to be pulled by the surgeon, resulting in thoracic duct injury and chylothorax formation. The other option of endovascular snare removal was thought to be not possible for the same reason.

Figure 1: left sided swelling over the neck, supraclavicular region and anterior chest wall after removal of Port-A-cath.
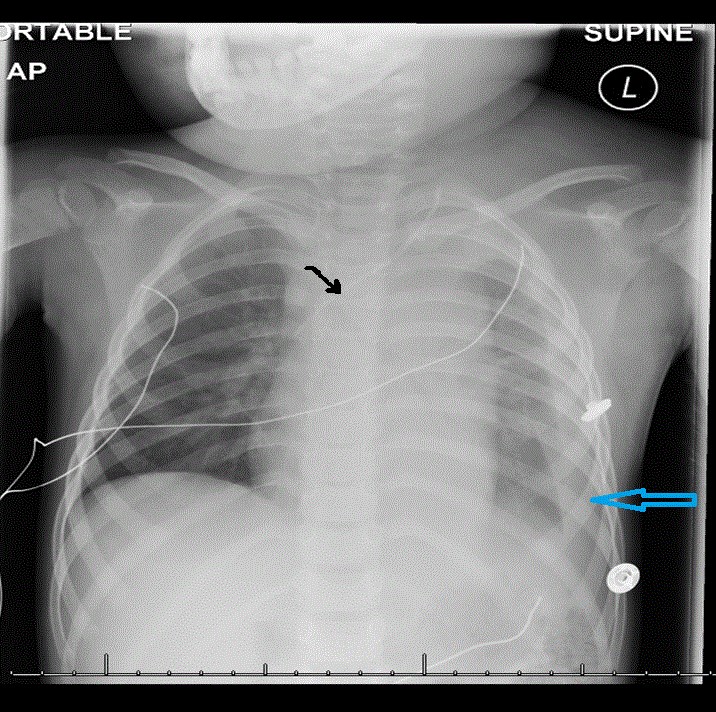
Figure 2: Chest X ray showing left sided pleural effusion (blue arrow) and retained part of central catheter (black arrow) along the brachiocephalic vein.
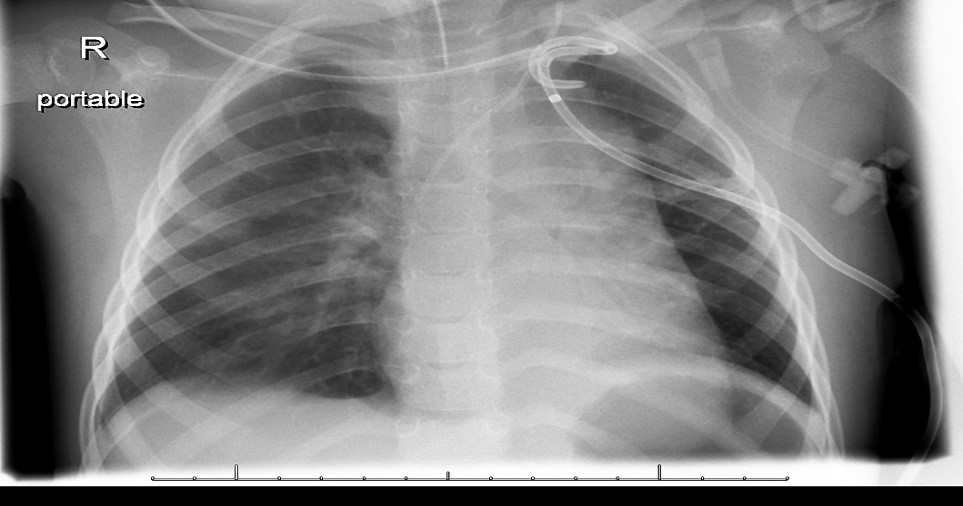
Figure 3: chest X ray after insertion of draining pigtail catheter.
Citation: Hanan Nazir (2019) Chylothorax Complicating Difficult Removal of Port-A-Cath in a Child with Acute Leukemia. Ann Pediatr Child Care: APCC-100010.