Annals of Pediatrics and Child Care
Case Report
Intermittent Suprasternal Neck Mass in Preterm Infant
Badawi MAS1*, Jassim FA2, Melhat AE¹, Zefov V3 and Dalwinder Singh1
1Department of Pediatrics, NICU, Latifa Women and Children hospital (LWCH), Dubai, (UAE)
2Department of Pediatric, Latifa Women and Children hospital (LWCH), Dubai, UAE
3Department of Radiology, Latifa Women and Children hospital (LWCH), Dubai, UAE
*Corresponding author: Mohamed Abou Seif Badawi, Department of Pediatric, Latifa Women and Children hospital (LWCH), Dubai, UAE, Tel: +00971507747459; Email: siefabusief@yahoo.com
Citation: Mohamed Abou Seif Badawi (2019) Intermittent Suprasternal Neck Mass in Preterm Infant. Ann Pediatr Child Care: APCC-100007.
Received date: 10 September, 2019; Accepted date: 17 September, 2019; Published date: 24 September, 2019
Abstract
The differential diagnosis of a neck mass in the pediatric age group is broad, extensive, and includes both serious and benign etiologies. Accurate diagnosis of a neck mass is critical as this will avoid unnecessary tests, radiation Exposure, biopsy and surgery. Here, we report a rare cause of neck swelling of a preterm baby who was admitted to NICU in Latifa women and children hospital (LWCH). We will discuss its diagnosis, association, differential diagnosis and the management.
Keywords: Neck swelling; Preterm; Thymus gland
Introduction
A premature female baby a product of non-consanguineous marriage weighing 0.7 kg was born at 26 week gestational age to P 0+2, 28 years old mother. Mother is Rubella immune with negative serology. Maternal antenatal ultrasound just before delivery was normal. Mother received two doses of betamethasone, had pregnancy induced hypertension on Aldomet and received Magnesium sulphate for premature delivery and high blood pressure. The miscarriages happened during the second trimesters without obvious cause.
Baby was delivered by LSCS through clear liquor. She cried immediately after birth with Apgar score of 6 and 8 at 1 & 5 minutes respectively. She was then hooked to NPIMV in view of poor respiratory effort and transferred to the neonatal intensive care unit (NICU) for further management.
In the NICU, she was intubated in view of increased oxygen requirement, worsening respiratory distress and given 1 dose of surfactant. She improved gradually and weaned successfully to non-invasive respiratory support then to room air. Trophic feeding was initiated early on day 3 of age then was upgraded gradually till reached full feed. She had initially unconjugated Hyperbilirubinemia of prematurity then neonatal cholestasis that was attributed to prematurity, total parenteral nutrition and an attack of neonatal sepsis with Klebsiella pneumoniae.
Once she started to grow, it was noticed that she had bilateral indirect inguinal hernia that was operated upon. She also had moderate sized umbilical hernia that was treated conservatively.
At post conception age of 3 months (corrected age 38 weeks), she was noted to have midline suprasternal swelling which bulges only with crying and during straining and disappears when she is at rest and comfortable. There were neither inflammatory signs on the overlying skin nor other swellings on neck examination (Figures 1-3).
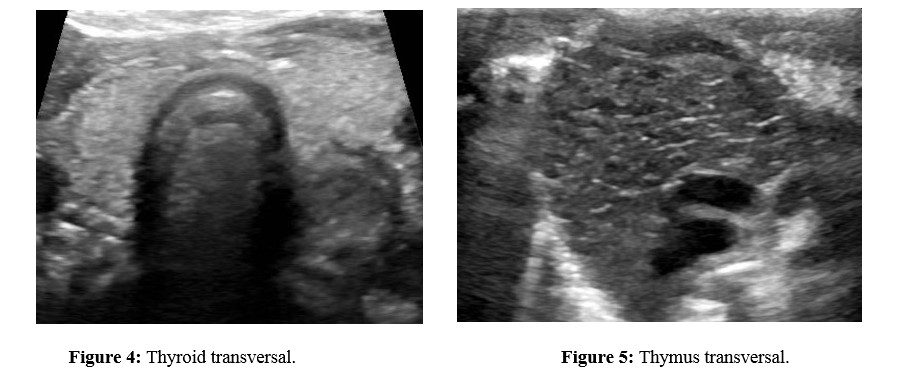
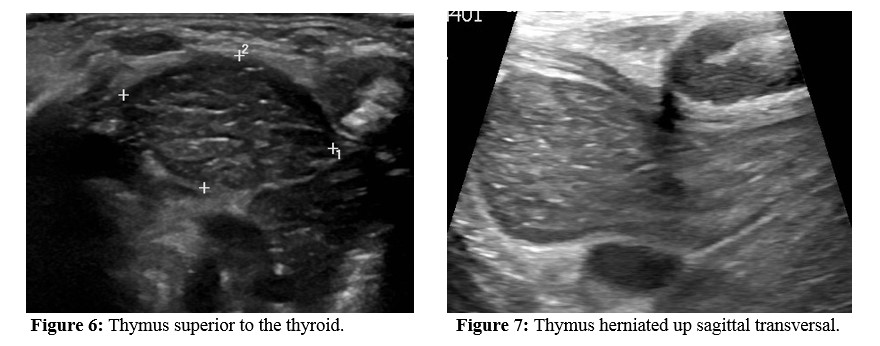
Neck ultrasound scan was done that confirm the diagnosis (Figure 4-7).
Neck Ultrasound was done that pick up the diagnosis.
Differential Diagnosis
The possible diagnoses of midline anterior neck mass include thyroglossal duct cyst, dermoid-epidermoid cyst, cystic hygroma, thyroid mass, and ectopic thymic mass [2]. As this swelling is evident only during crying (Valsalva’s maneuver) so all mentioned causes are ruled out.
There is only narrow spectrum of differential diagnosis for anterior neck swellings appearing during Valsalva’s maneuver which include jugular phlebectasia, apical lung herniation, Laryngocele and superior herniation of mediastinal thymus [3].
Jugular Phlebectasia refers to a congenital fusiform dilatation of the internal jugular vein without tortuosity. It is usually on the right but less commonly bilaterally. It appears as a soft compressible mass in the neck during straining. Apart from possible cosmetic deformity, the only reported complications are rare cases of thrombosis and Horner’s syndrome [4]. Clinically it would be located in a more lateral position (more commonly on the right), which could help to differentiate it from Thymic herniation. Sonography supplemented by Doppler examination accurately identifies the dilated internal jugular vein on Valsalva’s maneuver with venous blood flow [5]. This was clearly excluded on the Doppler ultrasound scanning in our case.
Apical/cervical lung hernia is defined as a protrusion of the lung apex into the cervical region through a deficiency in Sibson’s fascia and can be unilateral or bilateral. It is seen most often in the first 3 years of life and may resolve spontaneously. It typically presents as a compressible bulge in the supraclavicular region during crying or other procedures which increase intrathoracic pressure [6,7]. This was strongly excluded by clinical examination chest X ray and the ultrasound scanning in our case.
Laryngocele, an abnormal dilatation of laryngeal saccule, can occur in children but is more common in adult men in the fifth decade [8]. Laryngocele may be filled with air, fluid, pus, or a combination. Most are probably asymptomatic, but symptoms of breathlessness, cough, hoarseness and stridor may develop [9]. This has been excluded by the micro-laryngoscopy.
In our case, neck ultrasound scan showed intermittent superior herniation of the thymus and the sagittal ultrasound scan showed continuation of the thymus superiorly which is going up and down during Valsalva’s events (Figure 4-7).
Discussion
In our case the diagnosis was suspected clinically while observing the protrusion of the midline neck swelling during crying, straining, and it was confirmed by neck ultrasound as it was unusual to see such sign in this age group.
There are some reports regarding the association of thymic herniation with presence of inguinal hernia which is present in our baby in addition to the moderate size umbilical hernia. Our baby did not have any defect in the manubrium sterni which has been reported before in some cases [10].
After the diagnosis, the case had been reviewed with pediatric surgeon, pulmonologist, and otolaryngologist. In view of the benign nature of the lesion it was decided to continue on conservative treatment and to do micro-laryngoscopy to rule out Laryngocele.Micro-laryngoscopy showed mild congenital laryngomalacia with no other anomalies.
The thymus gland develops from the third pharyngeal pouch together with the inferior parathyroid glands at the fifth week of gestation. The developing encapsulated thymic primordia maintain its close relation with the parietal pericardium and descend with the pericardium during 7-8 weeks of gestation to assume its characteristic location in the superior anterior mediastinum anterior to the great vessels [11].
The thymus increases in size until puberty, where it can range from 30 to 40 grams. After puberty, there is gradual fatty involution that replaces the lymphoid components [12].
In newborns and infants, the normal thymus as well as its shape, size and location are readily visible at US and it has a typical, characteristic homogeneous and finely granular echo texture with some echogenic strands [2]. Therefore, ultrasonography should be the first imaging modality of choice. To our knowledge this is the 1st documented case in this age group with this diagnosis.
Conclusion
Baby remained stable and completely asymptomatic in room air. She was discharged home safely with outpatient clinic appointments. Parents were reassured about the benign nature of the lesion and the need to have close follow up of their baby.
On follow up she was still having the herniated suprasternal thymic mass with no evidence of any breathing or feeding difficulties. She continued to thrive, grow well and she did not require any surgical intervention .
Lessons for the Clinician
Author Disclosure
Dr. Badawi, El Melhat, Al Jassim, Zefov and Singh have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
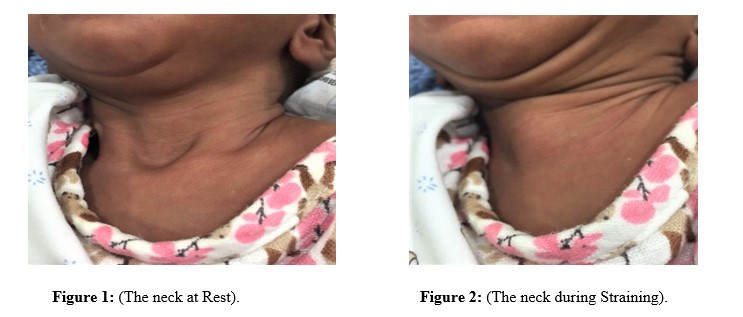

Figure 3: (The neck during Crying).
Citation: Mohamed Abou Seif Badawi (2019) Intermittent Suprasternal Neck Mass in Preterm Infant. Ann Pediatr Child Care: APCC-100007.