Emergency Medicine and Trauma Care Journal
Research article
Test the Termination of Regular Ischemic Premature Ventricular Contractions Variants with Nitro-glycerine; A new Therapeutic and Diagnostic Test; Retrospective Observational Study (14-Report Cases)
Elsayed YMH*
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
*Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt, Tel: +00201141292365, Email: dryaser24@yahoo.com
Citation: Elsayed YMH (2019) Test the Termination of Regular Ischemic Premature Ventricular Contractions Variants with Nitroglycerin; A new Therapeutic and Diagnostic Test; Retrospective Observational Study (14-Report Cases). Emerg Med Trauma Care J: EMTCJ-100004.
Received date: 15 July, 2019; Accepted date: 24 July, 2019; Published date: 05 August, 2019
Abstract
Background: Premature ventricular contractions are one of the most common cardiac arrhythmias. However, premature ventricular contractions are one of the manifestations of ischemic heart disease. Specifically, in coronary artery disease, the frequency and complexity of premature ventricular contractions are associated with mortality. Nitro-glycerine is one of the most useful anti-ischemic agents. Nitro-glycerine is a standard anti-ischemic agent. So why don’t use it as an antiarrhythmic in like-the current cases? But it is not known as anti-arrhythmic drug. Ischemic heart disease may be manifested and presented with ventricular arrhythmias like-premature ventricular contractions whatever the type.
Method of study and patients: My case study was an observational retrospective fourteen-case report series. The study was conducted in Fraskour Central Hospital; in both the Emergency Department and Intensive Care Unit. The author reported the fourteen-cases of variant regular ischemic premature ventricular contractions over nearly 12-months, started from July 1, 2018, and, ended on Jul 6, 2019.
Results: There are 35.71% of premature ventricular contractions-Bigeminy (5 cases), 28.75% of premature ventricular contractions-Trigeminy (4 cases), 14.28% of premature ventricular contractions-Quadrigeminy (2 cases), 14.28% of premature ventricular contractions-Pentageminy, (2 cases), and 7.14% of premature ventricular contractions-Hexageminy (1 case). With male predominance (64.29% vs. 35.71%), Mean age: 67.35 years (Median: 69, and Mode:75).
Conclusions: Regards the dramatic response of variant regular ischemic premature ventricular contractions to nitro-glycerine, it may be used as a new therapeutic and diagnostic antiarrhythmic agent in like-these cases.
Keywords: Nitro-glycerine; PVCs; Premature ventricular contractions; Test the termination; Variants of ischemic regular premature ventricular contractions
Abbreviations
AF : Atrial fibrillation
AMI : Acute myocardial infarction
CABG : Post-coronary artery bypass grafting
DM : Diabetes mellitus
ECG : Electrocardiography
HTN : Hypertension
ICU : Intensive care unit
IHD : Ischemic heart disease
IVI : Intravenous infusion
LBBB : Left bundle branch block
MI : Acute myocardial infarction
PD : Parkinson’s disease
PTCA : Percutaneous transluminal coronary angioplasty
Introduction
Historical bit: Until 2015, no new agents were developed in this field and the treatment of premature ventricular contractions with drugs has remained as something trivial for the past 20 years [1]. Historically, premature ventricular contractions (PVCs) were considered precursors of sudden cardiac death (SCD) and, for many years, their mere presence was taken as an indication for prescribing anti-arrhythmic agents [1].Recently, nitro-glycerine was introduced by the author as a newer antiarrhythmic agent in two case reports. The first reported case (2017) [2] was a case of ischemic premature ventricular contractions-bigeminy had shown a dramatic response to a trace dose of intravenous nitro-glycerine infusion. The second reported case (2019) [3] was another case of ischemic PVCs-quadrigeminy had shown a dramatic response to a trace dose of intravenous nitro-glycerine infusion.
Premature Ventricular Contractions; Scoping, Epidemiology, and Statistics: Generally, PVCs are the most common cardiac arrhythmia in patients with or without structural heart diseases (SHD) [4-8]. PVC is a type of arrhythmia characterized by premature heart contractions originating in one of the ventricles9. It is more prevalent with increasing age6. An estimated prevalence of premature ventricular contractions on standard 12-lead electrocardiography (ECG) was >1 PVCs /min occur in 1% to 4% of adult in the general population and 40% to 75% in 75% of healthy persons using on 24- to 48-hour Holter monitoring [5,10-14]. The prevalence of PVCs depends on the co-morbidities of the patients being screened and the duration of monitoring [15].
Definition, Description, and Regular Categorization:Premature ventricular contractions are characterized by premature and bizarre shaped QRS complexes that are unusually long (typically>120 msec) and appear wide on the ECG. The QRS complexes are not preceded by a P wave, and the T wave is usually large and oriented in a direction opposite the major deflection of the QRS [16].Traditionally, they have been thought to be relatively benign in the absence of structural heart disease but they represent an increased risk of sudden death in structural heart disease [10]. A premature ventricular contraction is caused by an ectopic cardiac pacemaker located in the ventricle [16].
Depending on whether there are one, two, or three normal beats between each PVC, the rhythm is called bigeminy, trigeminy, or quadrigeminy, etc [17]. The two beats are figuratively similar to two twins (hence Bi- ± Gemini) indicates the number (2) [18]. Tri-is a multiplier suffix indicating the number (3) [18]. Quadri-is a multiplier suffix indicating the number (4) [18]. Penta- is a multiplier suffix indicates the number (5) [18]. Hexa is a multiplier suffix indicates the number (6) [18]. Gemini is a prefix of is represented by the twins [19]. So, PVCs-Bigeminy means a cardiac arrhythmia in which every second beat is a ventricular premature complex (extrasystole) or one sinus beats between extra systoles. Trigeminy means a cardiac arrhythmia in which every third beat is a ventricular premature complex (extrasystole) or two sinus beats between extra systoles. Quadrigeminy means a cardiac arrhythmia in which every fourth beat is a ventricular premature complex (extrasystole) or three sinus beats between extra systoles [20]. Ventricular pentageminyis the occurrence of a premature ventricular contraction every the 5th beat or four sinus beats between extra systoles [17] (Figure 1).
Pathophysiology and Risk Factors: A premature ventricular contraction is a type of arrhythmia characterized by premature heart contractions originating in one of the ventricles9. PVCs are early depolarization of the myocardium originating in the ventricle10 caused by an electrical impulse or ectopic rhythm from any part of the ventricles, including the ventricular septum before the sinoatrial impulse has reached the ventricles [21]. PVCs is a common arrhythmia triggered by impulses arising outside the normal conduction pathway of the heart occurs even in people with no underlying heart disease (pre-existing heart condition, including angina pectoris, valve disease, or myocardial disease) [9]. PVCs often arise from a pre-excitation, mostly in the right ventricle4. A premature ventricular contraction is a sign of decreased oxygenation to the myocardium but is also found in healthy heart [22]. In most cases, premature ventricular contractions have a focal origin1. Suggested pathophysiological mechanisms for PVCs are re-entry, triggered activity, and enhanced automaticity [16].
Factors that increase the risk of premature ventricular contractions include male sex, advanced age, African-American race, hypertension underlying ischemic heart disease, bundle-branch block, hypomagnesemia, and hypokalaemia. The followings cause implicate in the presence of PVCs, Hypokalaemia, hypomagnesemia, acute myocardial infarction, ischemic heart disease, myocarditis, cardiomyopathy, myocardial contusion, mitral valve prolapse, hypoxia and/or hypercapnia, digoxin, sympathomimetic, tricyclic antidepressants, aminophylline, caffeine, cocaine, amphetamines, alcohol, tobacco, and hypercalcemia [16,23]. Required workup for premature ventricular contraction includes potassium levels, magnesium level, electrocardiography, and echocardiography 16. The optimal indications for therapy for premature ventricular contractions have not yet been elucidated [16].
Clinical Significance, Prognosis, and Mortality: Patients are usually asymptomatic [16]. The clinical significance of PVCs depends on their frequency, complexity, and hemodynamic response [16]. Ischemic heart disease may be manifested and presented with ventricular arrhythmias like-premature ventricular contractions whatever the type 2. The vast majority of patients with premature ventricular complexes are considered benign when they occur in patients without apparent SHD [24,25]. PVCs in patients without apparent SHD are safe once we rule out risk factors [24]. PVCs in patients with SHD are a marker of risk of SCD [24,26]. Previous studies using cohort showed that PVCs are associated with increased coronary heart disease (CAD) events and death [27]. Because PVCs are more likely to appear in the context of established CAD, they may be viewed as a marker of disease severity or as an endpoint in the natural history of the disease process [28]. In patients with CAD, PVCs have been shown to be associated with a poor prognosis [29,30]. Asymptomatic patients with frequent or complex PVCs have good prognosis 30. By extrapolation, it would appear that PVCs may confer some risk for ischemic stroke 27. Patients with PVCs are substantially more likely to develop subsequent coronary artery disease events and mortality compared with patients without PVCs [28]. The definition of high-frequency PVCs can vary from 10,000 to 20,000 PVCs/day based on the particular study consulted [26]. Frequent PVCs are associated with acute myocardial infarction (AMI) and SCD in patients without known CAD [31]. Some studies have found a significant risk of AMI and SCD associated with >30 PVCs per hour [31-33].
PVCs as a Precursor for Ventricular Tachycardia (VT) and Ventricular Fibrillation (VF): Ventricular tachycardia is the myocardial arrhythmias under His bundle branch and myocardial conduction fiber [21,34] defined ventricular tachycardia as more than 100 beats/min, and three or more consecutive spontaneous PVCs. Six or more rapid PVCs (frequency > 100/min) are considered as persistent VT (longer than 30 seconds), while less than 6 beats as non-persistent VT (episodes less than 30 seconds). Persistent VT is very dangerous, as it can trigger VF and SCD21. Patients with PVCs couplets are more prone to the development of VT than with single PVCs [35]. A higher PVCs-burden (> 26 %/day) is associated with LVD in patients without SHD [8,36].
PVCs-Induced Ventricular Dysfunction and Heart Failure: It has been reported that frequent PVCs can cause progressive LVD and dilation, which may be restored to normal after successful catheter ablation of the PVCs 8. Frequent PVCs are associated with the presence or subsequent development of left ventricular dilatation and dysfunction [37,38]. The evidence of this relation was that ablation of PVCs improved the LV dysfunction [39-43]. The mechanism responsible for PVCs-mediated LVD remains unclear [8]. Mechanisms proposed for PVCs-mediated LV dysfunction include alterations in calcium homeostasis, increased oxygen consumption, and ventricular dyssynchrony [8].
Management and Indications for Therapy: The most common indication for treating PVCs in the absence of structural heart disease (SHD) is the presence of symptoms that are not improved by reassurance [44,45]. Presence of symptoms in patients with structural heart diseases is considering primary indication. Elimination of high burden PVCs (10%) in patients with impaired LV function can be associated with significant improvement of LV function [41,42] even when significant scarring is present [46,47].
Antiarrhythmic Drugs and Their Controversies: Anti-arrhythmic drug treatment should be considered in case of frequent PVCs [4]. For patients without structural heart disease and mild symptoms, the first step in the treatment of patients with PVCs is reassurance 44. Studies have evaluated whether suppressing PVCs with antiarrhythmic agents improves prognosis [31]. Both Cardiac Arrhythmia Suppression Trials (CASTI: encainide and flecainide; CAST II: moricizine) showed that suppressing frequent PVCs significantly increased mortality in the treatment groups [48,49]. Treatment with a type Ic drugs (propafenone and flecainide) or a type III drug (sotalol, amiodarone, and dofetilide) vs catheter ablation. Treatment with class I or class III antiarrhythmic drugs always entails a small risk of proarrhythmia. The choice between drug therapy or ablation therapy is highly individualized [45].
Nitro-glycerine: Nitro-glycerine is the most common and oldest prescribed short-acting anti-anginal agent. Although the drug was introduced in clinical use since 1879, there remains an important need to educate both patients and health care providers on the various benefits of short-acting nitrates. Nitrates are vasodilators with predominant venous effects on large capacitance vessels. However, they increase coronary collateral circulation, increase aortic compliance and conductance and blood flow to ischemic areas of the myocardium. Nitrates alleviate anginal symptoms by directly influencing the coronary arteries, coronary collateral circulation, aortic compliance and conductance, and blood flow to ischemic areas of the myocardium [50]. Short-acting nitrates are beneficial in acute IHD [51]. Myocardial ischemia is the result of an imbalance between myocardial oxygen demand and myocardial oxygen supply. Despite nitro-glycerine clinically effective in the therapy of this condition, its exact mechanism of action is still uncertain [52]. Because of clinical observations suggesting that nitro-glycerine may suppress premature ventricular contractions during acute ischemia, a study was undertaken to assess the effect of nitro-glycerine on the incidence of PVCs in patients with acute myocardial infarction (AMI) [53]. Nitro-glycerine yield a significantly more rapid reduction in ventricular arrhythmias: 6 hours after onset of recording, the number of PVCs had declined to 39% of the baseline value [54]. Nitro-glycerine is one of the most useful anti-ischemic agents. IHD may manifest and presented with ventricular arrhythmias like- PVCs. Despite nitro-glycerine is not known as an antiarrhythmic drug but Suzanne B. and her fellows in reported that the clinical observations suggesting that nitro-glycerine may suppress PVCs during acute ischemia [55]. The corresponding author also reported a case of PVCs-bigeminy with a dramatic response of bigeminy to nitro-glycerine infusion [21]. The data indicate that nitro-glycerine may decrease the number of premature ventricular complexes for up to 3 hours in patients with AMI [56].
Nitro-glycerine is one of the most useful anti-ischemic agents [2]. But it is not known as anti-arrhythmic drug2. Because of clinical observations suggesting that nitro-glycerine may suppress premature ventricular complexes during acute ischemia, a study was undertaken to assess the effect of nitro-glycerine on the incidence of premature ventricular complexes in patients with acute myocardial infarction [52]. Recently, nitro-glycerine was introduced by the author as a newer antiarrhythmic agent in two case reports. The first reported case (2017) [2] was a case of ischemic PVCs-bigeminy had shown a dramatic response to a trace dose of intravenous nitro-glycerine infusion. The second reported case (2019) [3] was another case of ischemic PVCs-quadrigeminy had shown a dramatic response to a trace dose of intravenous nitro-glycerine infusion.
Case presentations
The author had reported fourteen-cases of variants of regular ischemic premature ventricular contractions through nearly 12-months, started from July 1, 2018, and, ended on Jul 6, 2019. The study was conducted in Fraskour Central Hospital; in both the Emergency Department and Intensive Care Unit. 60% of cases were male the remaining 40% were female. There was a different diagnosis for all cases. Otherwise, a case of PVCs-Hexageminy the remaining thirteen cases were admitted in the intensive care unit. The all the cases in the Intensive Care Unit (ICU) were undergone to treatment with nitro-glycerine IVI on dosing for about 30 minutes. ECG tracings were done before admission and 30 minutes after initiation the treatment with nitro-glycerine intravenous infusion (IVI) in very low dose (2.5mg/50 ml solvent, 7.5 ug/min) relatively for 30 minutes only as a therapeutic and diagnostic test [2]. Troponin test was positive in twelve cases. Thyroid function tests and electrolytes profile show no abnormalities. The echocardiographic reports showed evidence of IHD with variant regional wall motion abnormality according to the case. For more details, see (Table 1).
Case No 1: A 75-year-old painter, a heavy smoker, Egyptian married male patient presented to the Emergency Room with palpitations and dizziness. The printed ECG showed PVCs-Pentageminy. The patient gave a past history of anterior MI and hypertension (Figure 2 and 3).
Case No 2: A 63-year-old, Gov. officer, a heavy smoker, Egyptian male patient presented in the Emergency Department with angina. The printed ECG showed PVCs-Bigeminy. The patient gave a past history of IHD and hypertension (Figure 4).
Case No 3: A 67-year-old, carpenter, smoker, Egyptian male patient presented in the Emergency Department with angina and palpitations. The printed ECG showed PVCs-Quadrigeminy. The patient gave a past history of old MI, Atrial fibrillation (AF), and hypertension (Figure 5).
Case No 4: A 74-year-old, housewife, Egyptian female patient presented in the Emergency Department with angina. The printed ECG showed PVCs-Trigeminy. The patient gave a past history of recurrent angina and hypertension. (Figure 6).
Case No 5: A 91-year-old, retired, smoker, Egyptian male patient presented in the Emergency Department with dizziness and tremor. The printed ECG showed PVCs-Trigeminy. The patient is a Parkinson’s disease (PA). The patient gave a past history of hypertension (Figure 7).
Case No 6: A 75-year-old, worker, smoker, Egyptian male patient presented in the Emergency Department with palpitations. The printed ECG showed PVCs-Hexageminy. The patient gave a past history of old MI, AF, hypertension, and Post-coronary artery bypass grafting (CABG) (Figure 8).
Case No 7: A 58-year-old, worker, smoker, Egyptian male patient presented in the Emergency Department with angina. The printed ECG showed PVCs-Bigeminy. The patient gave a past history of diabetes and hypertension.
Case No 8: A 67-year-old, housewife, Egyptian female patient presented in the Emergency Department with palpitations. The printed ECG showed PVCs-Bigeminy. The patient gave a past history of IHD and hypertension.
Case No 9: A 67-year-old, Gov. officer, Egyptian female patient presented in the Emergency Department with angina. The printed ECG showed PVCs-Pentageminy. The patient gave a history of hypothyroidism continued on Eltroxin (100 ug per day), AF, IHD, and hypertension.
Case No 10: A 73-year-old, worker, smoker, Egyptian male patient presented in the Emergency Department with palpitations. The printed ECG showed PVCs-Quadrigeminy. The patient gave a past history of old MI, Left bundle branch block (LBBB), AF, hypertension, triple-vessels disease, and CABG.
Case No 11: A 50-year-old, housewife, Egyptian female patient presented in the Emergency Department with angina. The printed ECG showed PVCs-Trigeminy. The patient gave a past history of IHD and hypertension.
Case No 12: A 62-year-old, engineer, smoker, Egyptian male patient presented in the Emergency Department with palpitations. The printed ECG showed PVCs-Bigeminy. The patient gave a past history of IHD and hypertension.
Case No 13: A 67-year-old, housewife, Egyptian female patient presented in the Emergency Department with angina and palpitations. The printed ECG showed PVCs-Trigeminy. The patient gave a past history of recurrent angina and hypertension.
Case No 14: A 67-year-old, carpenter, smoker, Egyptian male patient presented in the Emergency Department with angina and palpitations. The printed ECG showed PVCs-Bigeminy. The patient gave a past history of recurrent angina, percutaneous transluminal coronary angioplasty (PTCA), and hypertension. For more details, see (Table 1).
Discussion and Results
The main complaint for the cases.
The percent of different arrhythmic diagnosis.
There are:
Ischemic evidence of PVCs in the study.
History: 92.86% (13 cases).
Clinical: 57.14% (8 cases).
ECG: 78.57% (11 cases).
Troponin test: 85.71% (12 cases) (Figure 13).
Outcome: 92.86% of cases (13 cases) had shown the dramatic response of variants of regular ischemic premature ventricular contractions to nitro-glycerine IVI within 30-minutes but the remaining 7.14% (1 case) also dramatic response but to nitro-glycerine transdermal skin-patch 10 (50mg) within 60-minutes. So, the total response was 100% but only with the delayed response in 7.14%.
Conclusion and Recommendations
My study report regards the variants of regular ischemic premature ventricular contractions indicating first a new described and managed arrhythmias. Testing the dramatic response of nitro-glycerine IVI on variants of regular ischemic premature ventricular contractions to differentiate the ischemic cause from the others. Regards the dramatic response of variants of regular ischemic premature ventricular contractions to nitro-glycerine, it may be used therapeutically and diagnostically as a new antiarrhythmic agent in like-these cases. Nitro-glycerine may have an indirect effect through increasing myocardial perfusion not due to documented clear antiarrhythmic effect. This test may decrease the overload uses of antiarrhythmic drugs and their adverse effects. It is recommended to widening the research area in the therapeutic effects of nitro-glycerine on irregular premature ventricular contractions.
Acknowledgment
I wish to thank Dr. Ameer Mekkawy; M.sc. for technical support and Critical Care Unit nurses who make extra ECG copy for helping me.
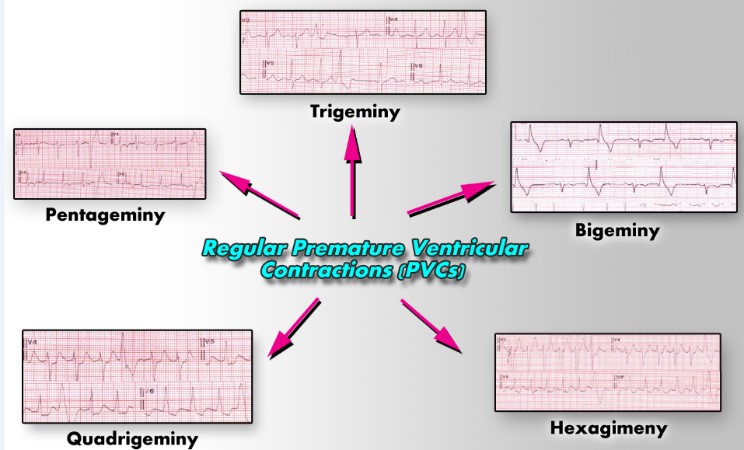
Figure 1: Showing variants of regular premature ventricular contractions.
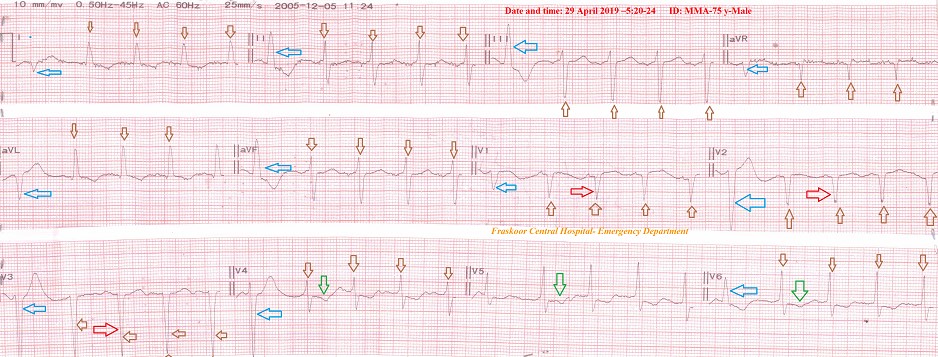
Figure 2: Case No. 1: ECG tracing of presentation A: showing PVCs-pentageminy through all ECG leads except technical artifact moved of lead V6 (blue arrows) with pathological Q wave in the leads; V1-3 (red arrows), ST wave depression in V4- 6 leads (green arrows), and intraventricular conduction defect. B: ECG strip showing pentageminy (blue arrows).
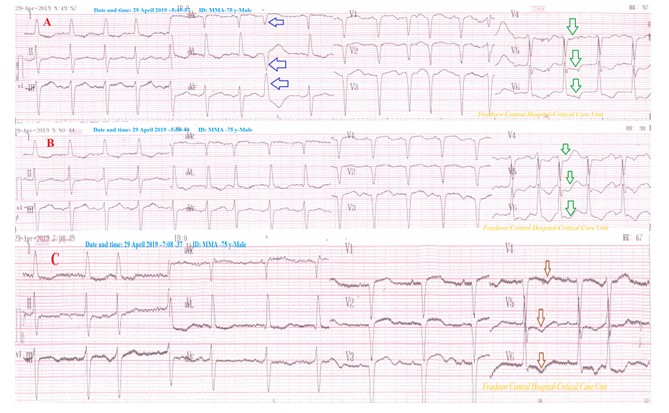
Figure 3: Case No. 1: ECG tracing was taken within 2 hours after nitro-glycerine IV Infusion. ECG tracing A strip showing still few PVCs-pentageminy (blue arrows) with ST-segment depressions in V4- 6 leads (green arrows) and persistent pathological Q wave in V1-3 leads. ECG tracing B: ECG strip showing still ST-segment depressions in V4- 6 leads (green arrows) and persistent pathological Q wave in V1-3 leads. ECG tracing C strip showing nearly complete disappearance above all ECG abnormalities but still T-wave inversion in V4-6 (brown arrows).
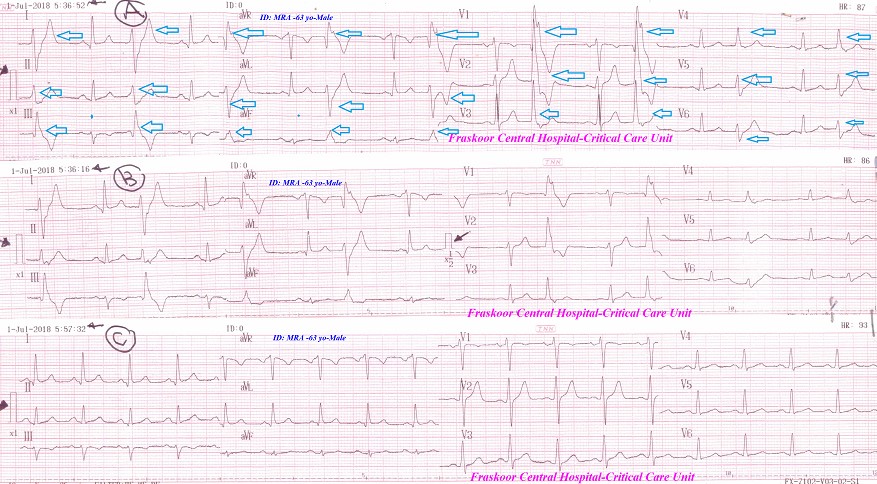
Figure 4: Case No. 2: ECG tracing A showing PVCs-bigeminy through all ECG leads (blue arrows). ECG tracing B (halve calibration) showing like-tracing A. ECG tracing C after NTG IVI showing complete disappearance of all above bigeminy.
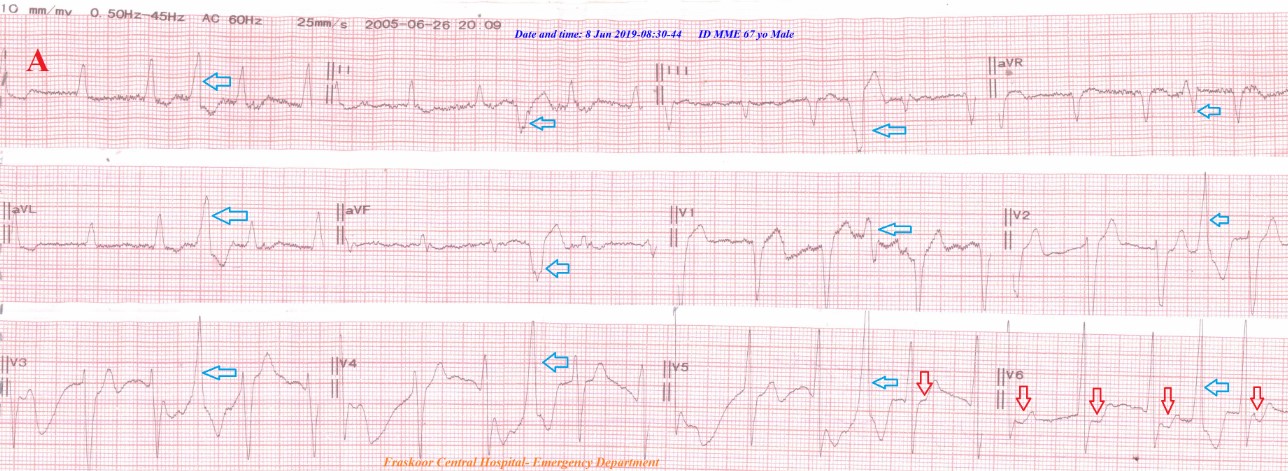
Figure 5: Case no 3 ECG tracing A showing PVCs-Quadrigeminy (blue arrows). ST-segment depressions in V5- 6 leads (red arrows). ECG tracing B after NTG IVI showing complete disappearance of all above Quadrigeminy, there is evidence of IHD with ST-segment depressions in I, aVL, V3- 6 leads (red arrows) pathological Q-wave in V1-2 (old MI) (green arrows) and AF more clear.
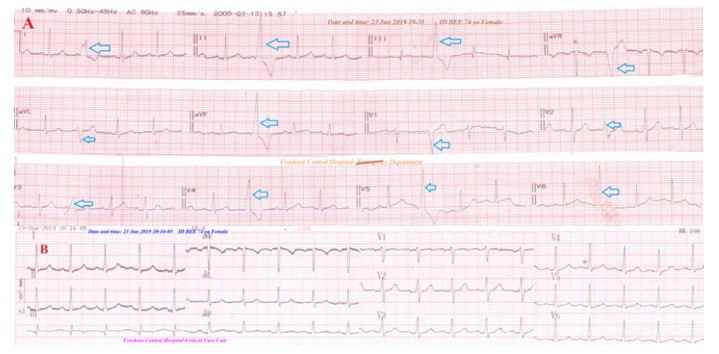
Figure 6: Case no 4: ECG tracing A showing PVCs-Trigeminy through all ECG. (blue arrows). B-ECG tracing after NTG IVI showing complete disappearance of all above Trigeminy.
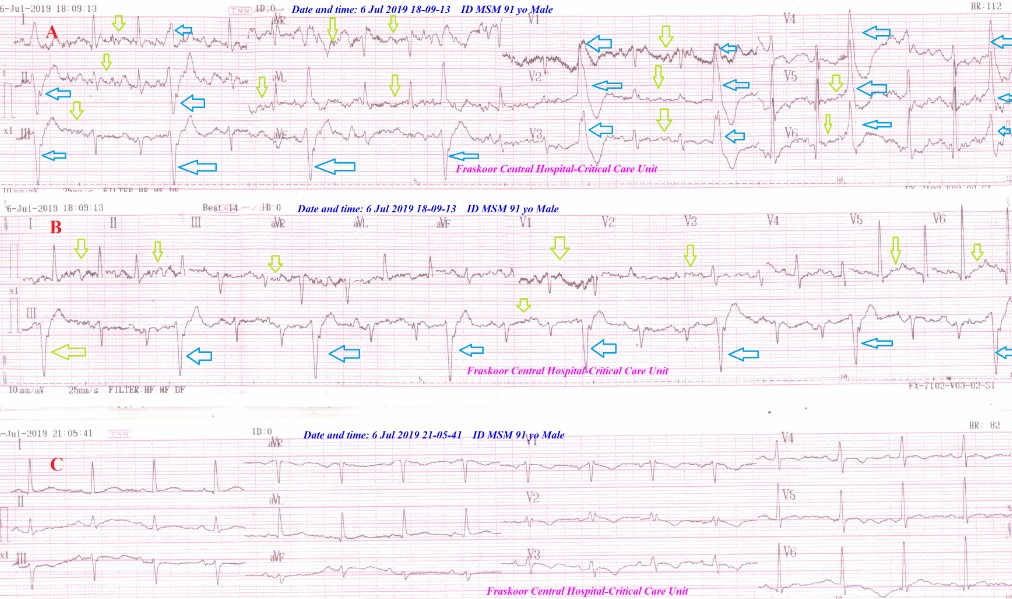
Figure 7: Case no 5: ECG tracing A showing PVCs-Trigeminy through all ECG. (blue arrows), artifacts of PD tremor (lemon arrows). ECG tracing B strip after NTG IVI showing the same B-ECG tracing. ECG tracing C after NTG IVI was taken during sleep (no tremor) showing complete disappearance of all above Trigeminy.
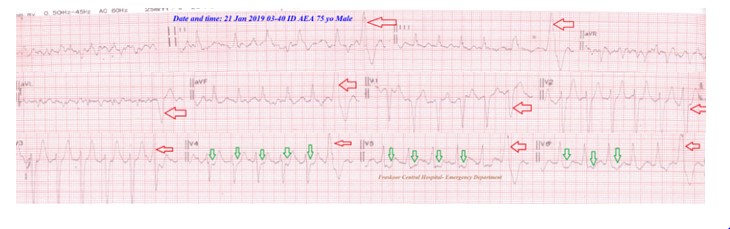
Figure 8: Case no 6: A-ECG tracing showing PVCs-Hexageminy through most of ECG leads (red arrows) with ST-segment depressions in V4-6 leads (green arrows).
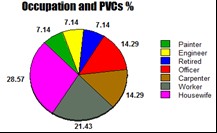
Figure 9: Showing effects of occupations on PVCs %.
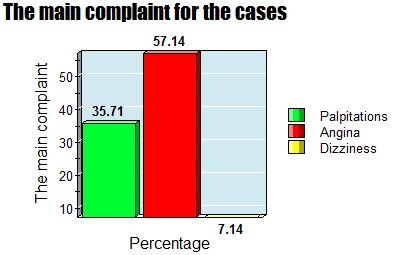
Figure 10: Showing the main complaint for the cases.
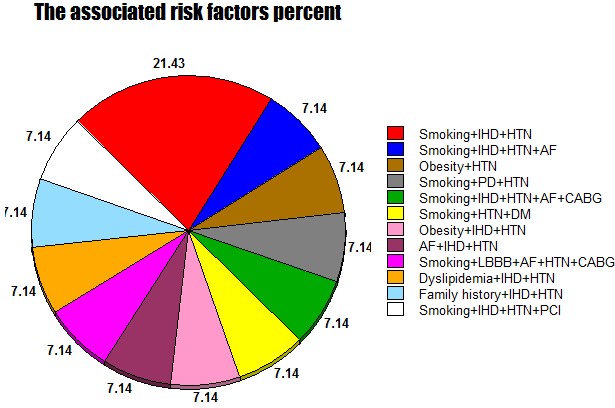
Figure 11: Showing the percent of associated risk factors.
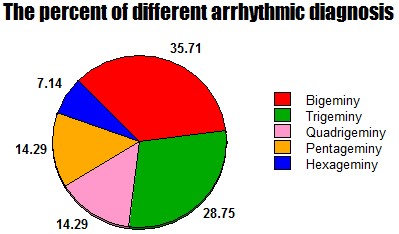
Figure 12: Showing the percent of different arrhythmic diagnosis.
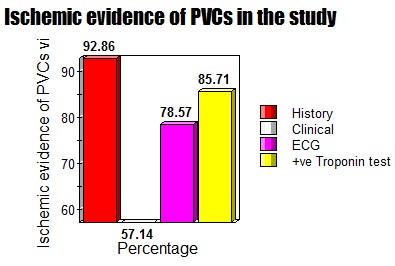
Figure 13: Showing ischemic evidence of PVCs in the study.
|
Case No.
|
Age |
Sex |
Occupation |
The main complaint |
BP mg Hg |
Pulse bpm |
RR |
O2 Sat. % |
Associated RF |
Arrhythmic diagnosis |
Outcome |
|
|
1 2 3 4 5 6 7 8 9 10 11 12 13 14 |
75 63 67 74 91 75 58 62 45 73 50 62 77 71 |
M M M F M M M F F M F M F M |
Painter Gov.officer Carpenter Housewife Retired Worker Worker Housewife Gov.officer Worker Housewife Engineer Housewife Carpenter |
PalpitationsAngina AnginaAngina Dizziness PalpitationsAngina Palpitations Angina Palpitations Angina Palpitations Angina Angina |
170/100 150/90 160/110 150/90 160/110 170/100 140/100 180/90 160/90 150/80 160/110 150/90 170/90 160/110 |
94 88 74 90 110 150 75 60 82 78 88 160 95 90 |
14 18 16 13 19 12 16 16 18 18 14 20 16 14 |
96 97 96 98 97 97 95 98 94 96 96 97 94 98 |
Smoking,IHD, HTN Smoking,IHD, HTN Smoking,IHD,HTN,AFObesity,HTN Smoking,PD,HTN Smoking,IHD,HTN,AF,CABGSmoking,HTN,DM Obesity,IHD,HTN AF,IHD,HTN AF,IHD,HTNDyslipidemia Dyslipidemia,IHD,HTN Family history,IHD,HTN Family history,IHD,HTN Smoking,IHD,HTN,PTCA |
Pentageminy Bigeminy Quadrigeminy Trigeminy Trigeminy Hexageminy Bigeminy Bigeminy Pentageminy Quadrigeminy Trigeminy Bigeminy Trigeminy Bigeminy |
Dramatic response all cases after initiation the treatment with nitroglycerin IVI in very low dose (2.5mg/50 ml solvent,7.5 ug/min) |
|
Table 1: Summary of the History, Clinical, and Management Data for the Study Cases.
Citation: Elsayed YMH (2019) Test the Termination of Regular Ischemic Premature Ventricular Contractions Variants with Nitroglycerin; A new Therapeutic and Diagnostic Test; Retrospective Observational Study (14-Report Cases). Emerg Med Trauma Care J: EMTCJ-100004.