Emergency Medicine and Trauma Care Journal
Research Article
Clinical Factors Affecting Mortality in Patients with Traumatic Shock Caused by Road Traffic Accidents Admitted to the Emergency Department: A Prospective Cohort Study
Ton Thanh Tra1*, Pham Thi Ngoc Thao1, Nguyen Van Khoi1, Le Quoc Hung1, Koji Wada2, Anthony FT Brown3
1Cho Ray Hospital, Ho Chi Minh City, Vietnam
2International University of Health and Welfare, Tokyo, Japan
3Faculty of Medicine, University of Queensland, Queensland, Australia
*Corresponding author: Ton Thanh Tra, Cho Ray Hospital, Ho Chi Minh City, Vietnam, Tel: +84903673451, Email: tonthanhtra@yahoo.com
Citation: Ton Thanh Tra, Thao T.N Pham, Van Khoi N, Quoc Hung L, Wada K, et al. (2019) Clinical Factors Affecting Mortality in Patients with Traumatic Shock Caused by Road Traffic Accidents Admitted to The Emergency Department: A Prospective Cohort Study. Emerg Med Trauma Care J: EMTCJ-100002.
Received date: 08 July, 2019; Accepted date: 15 July, 2019; Published date: 22 July, 2019
Abstract
Background: Trauma is a leading cause of death in the young population in Vietnam, especially among patients with traumatic shock. This study was performed to identify the clinical factors that can be used to predict early mortality (within the first 24 hours after admission) and in-hospital mortality (within 30days) in patients with traumatic shock caused by road traffic accidents in an emergency department in Vietnam.
Methods: A prospective observational cohort study was performed at the Emergency Department of Cho Ray Hospital, Ho Chi Minh City, Vietnam from June 2018 to December 2018. All patients who had been involved in road traffic accidents and developed traumatic shock (systolic blood pressure of <90 mmHg) within 24 hours of admission were enrolled. The clinical factors upon admission were collected, and the patients were followed up for 24 hours after admission and until day 30 or discharge to calculate early mortality and in-hospital mortality, respectively. Univariate and multivariate logistic regression analyses were performed to identify mortality-related factors.
Results: In total, 326 patients were enrolled (mean age, 37.6 ± 15.4 years). The early and in-hospital mortality rates were 29.4% and 47.5%, respectively. The univariate and multivariate logistic regression showed that a Glasgow coma scale (GCS) score of ≤ 8 and systolic blood pressure (SBP) of ≤ 50 mmHg were associated with early mortality (odds ratio [OR] =25.0, 95% confidence interval [CI]=7.50-83.6 and OR=3.11, 95% CI=1.34-7.18, respectively). A GCS score of ≤ 8, SBP of ≤ 50 mmHg, and Injury Severity Score (ISS) of ≥ 25 were associated with in-hospital mortality (OR=20.9, 95% CI= 9.75-44.8; OR=3.16, 95% CI=1.05-5.20; and OR=2.21, 95% CI=1.58-3.10, respectively).
Conclusions: A GCS score of ≤ 8 and SBP of ≤ 50 mmHg were associated with early mortality and a GCS score of ≤ 8, SBP of ≤ 50 mmHg, and ISS of ≥ 25 were associated with in-hospital mortality among patients with traumatic shock caused by road traffic accidents.
Keywords: Clinical factors; Mortality; Road traffic accidents; Traumatic shock
Abbreviations
AIS : Abbreviated Injury Score;
CI : Confidence interval;
CT : Computed tomography;
ED : Emergency Department;
GCS : Glasgow coma scale;
GAP score : Glasgow coma scale, age, systolic blood pressure score;
ISS : Injury Severity Score;
MGAP score : Mechanism, Glasgow coma scale, age, and arterial pressure score;
OR : Odds Ratio;
SBP : Systolic Blood Pressure
Introduction
Trauma is the leading cause of death among individuals aged 1 to 44 years worldwide [1,2]. According to the 2013 statistics of the World Health Organization, road traffic accidents were the ninth leading cause of death worldwide, accounting for 24% of injury-related deaths, and are predicted to be the fifth leading cause of death by 2030 [3]. The World Health Organization estimated that road traffic accidents resulted in the death of 1.2 million people and the injury of 20 to 50 million people worldwide. More than 90% of deaths occurred in low- and middle-income countries [3]. According to the World Bank, the cost of accidents is almost 2% of the gross domestic product of low- and middle-income countries, resulting in massive losses to their economies by road traffic accidents [3].
Vietnam has a high incidence of traffic accidents. According to the Vietnam National Traffic Safety Committee, about 10,000 people die and another 30,000 people are injured annually due to traffic accidents in Vietnam. Many efforts have been made to reduce the incidence of road traffic accidents, but the number of such accidents remains high and is still a health, social, and economic problem in Vietnam and other developing countries. In our daily practice, many patients present with shock or multiple injuries caused by road traffic accidents and require triage, resuscitation or transfer.
Many advances have been made in pre-hospital care, emergency care, resuscitation, and bleeding procedures during the last few decades; however, the mortality rate among patients with traumatic shock or multiple trauma remains as high as 25% to 54% [2,4-7]. Additionally, many biomarkers, laboratory findings, and clinical factors have been researched with respect to their relationship to mortality in patients with trauma. Trauma scores have also been developed to predict injury severity and mortality in patients with all types of traumatic injury. However, these factors were developed and validated in select patient populations.
In our daily practice, more than 80% of patients with trauma are young (<40 years old), have been injured in road traffic accidents, and are male. The present study was based on the following question: What are the clinical factors affecting mortality in patients with traumatic shock caused by road traffic accidents who are admitted to the Emergency department (ED) of Cho Ray Hospital? Identification of these clinical factors affecting mortality will support physicians in triage, resuscitation, and transfer of patients as well as consultation with patients’ families in daily clinical practice. The aim of this study was to determine which clinical factors are related to early mortality and in-hospital mortality in a population of patients with traumatic shock caused by road traffic accidents admitted to an ED, Ho Chi Minh City in Vietnam.
Materials and Methods
Study design: This prospective single-center cohort study was conducted atCho Ray Hospital in Ho Chi Minh City, Vietnam. Cho Ray is a tertiary teaching hospital with 2,800 beds, a 72-bed ED, and an annual census of more than 100,000 emergency patients. Approximately 20% to 25% of patient presentations to the ED were due to trauma. A life-saving operation room is set up in the ED to be used for severely bleeding patients with traumatic shock who cannot be transferred to the operating theatre. An ultrasound machine, X-ray machine, computed tomography (CT) scanner, electrocardiograph, ventilators, biochemistry point-of-care machines, and other medical equipment are available in the resuscitation area. Two senior emergency doctors and four registered nurses work by shifts in the resuscitation bay. Patients with traumatic shock are triaged as the first priority and treated in the resuscitation area of the ED. The Advanced Trauma Life Support protocols are used in resuscitation, procedures, and nursing care.
Patient inclusion and exclusion criteria: Patients with traumatic shock (defined as systolic blood pressure [SBP] of <90 mmHg within 24 hours of admission) who presented to our ED from 1 June 2018 to 31 December 2018 were enrolled in this study. Patients were excluded if they had undergone an emergency operation before admission to Cho Ray Hospital, were pregnant, had significant chronic disease prior to injury, or were pulseless upon arrival.
Data collection: The patients’ vital signs were measured upon arrival. The SBP, diastolic blood pressure, respiratory rate, pulse rate, pulse oximetry, body temperature, and Glasgow coma scale (GCS) score were measured by the triage nurse. Blood samples were collected after the primary assessment. If needed, ultrasound, X-ray, and CT examinations were performed using the machines in the ED. The Injury Severity Score (ISS) was evaluated by the emergency doctors. Patients were followed up for 24 hours after admission and until day 30 or discharge to calculate early mortality and in-hospital mortality, respectively.
Statistical methods: Student’s t-test and the Mann–Whitney test were used to determine the significance of differences between the survival and non-survival groups. Univariate and multivariate logistic regression analyses were performed to identify factors related to early mortality and in-hospital mortality. Significant differences were identified when p < 0.05.
Ethics: The research protocol was approved by the Ethics and Scientific Committee of Cho Ray Hospital (N669/CRH, dated 20/6/2018). The patients’ relatives provided written informed consent for the patients’ participation in this research.
Results
In total, 22.799 patients with trauma were admitted to the ED during the study period. Of these patients, 326 with shock caused by road traffic accidents were enrolled.
Discussion
This study was performed to determine which clinical factors affected early mortality and in-hospital mortality in patients with traumatic shock caused by road traffic accidents. This prospective cohort study involved 326 patients with traumatic shock admitted to an ED in Vietnam. The results showed that a GCS score of ≤ 8 and SBP of ≤ 50 mmHg were associated with early mortality and that a GCS score of ≤ 8, SBP of ≤ 50 mmHg, and ISS of ≥ 25 were associated with in-hospital mortality.
The patients who had been injured in road traffic accidents in the present study were primarily young and male. In total, 90.4% of patients were <60 years old, and 79% of patients had been involved in motorbike accidents [8] analyzed data from 2013 to 2015 in Ho Chi Minh City and found that the number of accidents, deaths, and injuries involving young people substantially worsened (increased by 260%). Many factors were associated with these increases. The main factor is that the number of motorcycles and mopeds on the road increased by 28,515,968 vehicles (153.2%) from 2006 to 2016 [9]. The number of motorcycles as a proportion of all motorized vehicles is highest in Vietnam among all Asian countries.
The mortality rate among patients with traumatic shock is very high. In the present study, the early mortality rate was 29.4% and in-hospital mortality rate was 47.5%. In comparison, a study by [10] involving 252 Korean patients with traumatic shock showed an early mortality rate of 11.9% and in-hospital mortality rate of 32.9%. These mortality rates are much lower than our results. The difference can be explained by the fact that our patients had very severe injuries (SBP=60.7 ± 22.3 mmHg, GCS score=7.0 (3.0-14.0), ISS=21.5 ± 5.6, and incidence of traumatic brain injury=61.7%) (Table 1). Another research done [11] evaluated 219 patients with traumatic shock and found that the mortality rate at 28 days after admission was 36%. Their study was performed in the United States and Europe, and their population comprised patients with traumatic hemorrhagic shock; those with traumatic brain injury were excluded. In clinical practice, however, traumatic brain injury cannot be definitively excluded at the time of admission. In the present study, 61.7% of patients with traumatic shock had traumatic brain injury, and most patients died of this traumatic brain injury within the first 24 hours after admission.
Because of the high volume of patients with trauma, clinicians at our institution felt that they needed a trauma score that was easy and simple yet accurate and could be applied at the scene of an accident or upon arrival to our ED. The results of our study show that two simple clinical factors (GCS score and SBP) can be used to predict early mortality. Similar results were reported by [12] in Iran; in their study, a GCS score of ≤ 8 was associated with hospital mortality in cases of pedestrian injury (OR=72.24, 95% CI=23.19-225.05). In 2015, [13] evaluated 220 patients with multiple trauma in the United Arab Emirates (91.6% were aged <60 years, the male: female ratio was 3.7:1.0, and the mortality rate was 40%). They found that the MGAP score was a better predictor than the Revised Trauma Score in the mild and moderate risk groups; in the high risk group, however, the MGAP score and Revised Trauma Score had the same value for prediction of in-hospital mortality [13]. However, our trauma population was young; most of the patients were ?60 years old. Moreover, in our clinical practice, an SBP of 90 mmHg is used as the cutoff for triage, resuscitation, and transfer of patients with traumatic shock.
In our patient cohort, most patients had been involved in motorbike accidents. Although most trauma scores do not typically affect the initial clinical decision-making process, an appropriate score may positively influence care such that greater attention and human resources are focused on the most severely injured patients within the “golden hour,” which is so vital to patient survival. Our data show that the GCS score and SBP at admission were the clinical factors associated with early mortality; age and sex were not associated. The reason for this finding is that our population was young (95% were aged ?60 years) and 77% were male.
Patients with traumatic shock need every available resource applied to their resuscitation in a timely and efficient manner. The decision to allocate these resources is easier when a readily applicable trauma score can be calculated, and a clinical decision made for each patient. The GCS score and SBP are very simple and easy-to-calculate clinical factors for patients presenting to E.Ds. Furthermore, our study clearly shows that these factors can be used to accurately predict the mortality of Vietnamese patients with traumatic shock caused by road traffic accidents. When the GCS score was ≤ 8, the risk of early mortality was 25.03 times higher and that of in-hospital mortality was 20.90 times higher. Similar findings were reported [14] in Iran; they showed that a GCS score of≤8 was an independent factor for mortality prediction [15] studied 202 patients with traumatic shock in the United Arab Emirates in 2013, among whom 72.3% of injuries were caused by road traffic accidents, and found that a GCS score of 5.5 and ISS of 13.5 were the best mortality predictors. Another study by [16] in Spain in 2015 showed that a GCS of ≤8 was a mortality predictor (OR=13.52, 95% CI=5.81-31.45).
The Trauma Score was first described in 1981 by Champion et al. to develop a simpler scoring system that enabled assessment during pre-hospital care or triage. This score initially comprised the GCS score, respiratory rate, SBP, respiratory expansion, and capillary refill [17]. The Revised Trauma Score was described by the same authors in 1989 and excluded respiratory expansion and capillary refill because these parameters are difficult to assess in the field [18]. The mechanism, GCS, age, and arterial pressure (MGAP) score was derived and validated among a French population, and it was first described by Sartorius et al. [19] in 2010. A simplified version called the GAP score was described by [19] in 2011 and eliminated the mechanism score from the MGAP score. They performed a prospective multicenter study of a Japanese population and found the GAP score to be an accurate predictor of in-hospital mortality. The GAP score combines the GCS score (3-15), age (<60 years: 3 points, ≥ 60 years: 0 points), and SBP (?60 mmHg: 0 points, 60-120 mmHg: 3 points, and ?120 mmHg: 6 points). Our data shows clearly that GCS and SBP but not age were the related factors to mortality. That means the GAP score may not be used for mortality prediction to these populations.
Many international guidelines currently suggest that permissive hypotension may offer a survival benefit over conventional resuscitation for patients with traumatic shock. The SBP was referred at different levels from 50 to 100 mmHg in permissive hypotension resuscitation. Permissive hypotension may additionally reduce the blood loss volume and requirement for blood transfusion [21,22]. In the present study, a low SBP at admission was a predictor for early mortality and in-hospital mortality. When the SBP was at 51-70 mmHg, the risk for early mortality was 2.12 (95% CI= 1.02-4.39) but when the SBP ≤ 50 mmHg, the risk of early mortality was 3.11(95% CI=1.34-7.18) (Table 3). The risk of in-hospital mortality was 2.19 (95% CI=0.90-4.59) when SBP=51-70 mmHg and was 3.16 (95%CI=1.05-5.20) when SBP ≤ 50 mmHg (Table 4). The data clearly showed that a severely low SBP results in worse outcomes in patients with traumatic shock with or without traumatic brain injury.
The risk factors for patients with trauma can be classified into three categories: anatomical severity, physiological severity, and patient reserve. Anatomical severity describes the degree of anatomical derangement and can be measured by the ISS or New ISS. In 1974, Backer et al introduced the ISS, which arose from the need for a simple and easy scoring system that was reliably correlated with trauma morbidity and mortality using the highest AIS severity score in each of the three most severely injured body regions [23]. Our research showed that the ISS was a predictor if in-hospital mortality. Patients with an ISS of ≥ 25 had a 2.21 higher risk than those with an ISS of ?16. However, evaluation of the ISS is more time-consuming, and CT scan or operation results are sometimes needed.
Traumatic shock is very severe condition, and treatment must be initiated with in the “golden hour” to save the patient’s life. Simple prognostic predictors should be used during pre-hospital care or at ED admission. Our data shows that GCS, SBP and ISS were the related factors for early mortality and in-hospital mortality in traumatic shock patients caused by road traffic accidents. These clinical factors could be used during pre-hospital care or at ED triage.
With respect to the time of death after injury, 61.9% of total deaths occurred within the first 24 hours after admission in the present study. More than 95% of patients died within the first 7 days. After the first week from admission, less than 5% patients died (only 5 patients died from days 10 to 30) (Figure 1). Similar results were found by [24] in the United States in 2016. They evaluated 1566 patients with pelvic trauma and found that the early mortality rate was 9.96% but that 57.0% of the total deaths occurred within the first 24 hours of admission, 20% died after 7 days of hospitalization, and a significantly low percentage of patient deaths were caused by in-hospital or trauma -related complications [24]. These findings imply that the resuscitation procedures and critical care were of high quality and saved patients’ lives during the treatment period. Figure 1 shows that 61.9% of all deaths occurred within the first 24 hours after admission. More than 95% of patients died within the first 7 days, and less than 5% died after the first week from admission.
In the 40th-50th of previous century, patients with trauma died in a trimodal distribution (on-site mortality, early mortality, and late mortality). During the last few decades, the proportions of deaths occurring within the first few minutes or hours of injury have not changed, but late deaths due to multiple organ failure and sepsis have declined dramatically. This has shifted the trimodal distribution to a bimodal distribution death of patients with trauma [25-27]. Our results show that the death of patients with trauma exhibits a bimodal distribution, as in other studies.
Limitation
Our study has the following limitations. First, the GCS score may be difficult to evaluate and monitor in patients with toxicities, such as those who have been drinking alcohol, and may be different between evaluators. Second, the study was performed at a tertiary teaching hospital containing a trauma center with a high level of human resources and medical equipment. The generalizability of our findings to all Vietnamese hospitals may be limited. However, several other hospitals have similar levels of equipment, facilities, and trauma volume in Vietnam and could potentially apply our findings to their practice. Further multicenter research is required to fully assess these factors.
Conclusion
Our analysis showed that a GCS score of ≤ 8 and SBP of ≤ 50 mmHg (but not the ISS) were associated with early mortality and that a GCS of ≤ 8, SBP of ≤ 50 mmHg, and ISS of ≥ 25 were associated with in-hospital mortality in patients with traumatic shock caused by road traffic accidents.
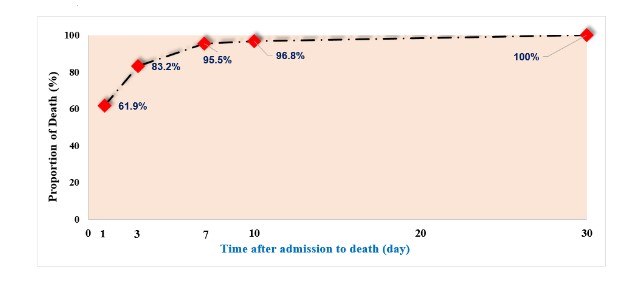
Figure 1: Time to death after admission (n=155).
|
Variables |
Results |
|
Age (mean ± SD, year) |
37.6 ± 15.4 |
|
Gender |
- |
|
Male (n, %) |
252 (77.3% |
|
Female (n, %) |
74 (22.7%) |
|
Traumatic brain injury (n, %) |
201 (61.7%) |
|
Non traumatic brain injury (n, %) |
125 (38.3%) |
|
Heart rate (mean ± SE, b/m) |
101.8 ± 25.3 |
|
SBP(mean ± SE, mmHg) |
60.7 ± 22.3 |
|
RR (median, IQR, time/m) |
18 (0-20) |
|
GCS score (median,IQR) |
7.0 (3.0-14.0) |
|
ISS (mean ± SE) |
21.5 ± 5.6 |
|
Early mortality (n, %) |
96 (29.4%) |
|
In-hospital Mortality (n, %) |
155 (47.5%)
|
|
Note:SBP, systolic blood pressure; RR, respiratory rate; GCS, Glasgow coma scale; |
|
|
ISS, Injury Severity Score; SE, standard error; IQR, interquartile range |
|
Table 1: shows the patients’ characteristics. Their mean age was 37.6 ± 15.4 years, and the male: female ratio was 3.4:1.0. A total of 61.7% patients had traumatic brain injury. The mortality rate in the first 24 hours after admission (early mortality) was 29.4%, and the 30-day mortality rate (in-hospital mortality) was 47.5%.
|
- |
Total n=326 (%) |
- |
Early Mortality n=96, (%) |
p |
In- hospital Mortality n=155, (%) |
P |
|
Age (year) <25 |
- |
- |
- |
- |
- |
- |
|
- |
89 (27.3) |
- |
27 (30.3) |
0.99 |
40 (44.9) |
0.54 |
|
25-34 |
71 (21.8) |
- |
21 (29.6) |
- |
31 (43.7) |
- |
|
35-46 |
81 (24.8) |
- |
23 (28.4) |
- |
44 (54.3) |
- |
|
≥ 47 |
85 (26.1) |
- |
25 (29.4) |
- |
40 (47.0) |
- |
|
GCS score |
||||||
|
3-8 |
185 (56.7) |
- |
88 (47.6) |
<0.001 |
136 (73.5) |
<0.001 |
|
9-13 |
55 (16.9) |
- |
5 (9.1) |
- |
8 (14.5) |
- |
|
14-15 |
86 (26.4) |
- |
3 (3.5) |
- |
11 (12.8) |
- |
|
ISS |
||||||
|
< 16 |
95 (29.1) |
- |
23 (24.2) |
0.54 |
31 (32.6) |
0.002 |
|
16-24 |
185 (56.8) |
- |
60 (32.4) |
|
97 (52.4) |
- |
|
≥ 25 |
46 (14.1) |
- |
13 (28.2) |
|
27 (58.7) |
- |
|
SBP (mmHg) |
||||||
|
80-89 |
- |
53 (16.2) |
27 (50.9) |
<0.001 |
34 (64.2) |
0.008 |
|
71-79 |
- |
98 (30.1) |
33 (33.7) |
- |
52 (53.1) |
- |
|
51-70 |
- |
75 (23.0) |
16 (21.3) |
- |
31 (41.3) |
- |
|
≤ 50 |
- |
100 (30.7) |
20 (20.0) |
- |
38 (38.0) |
-
|
|
Note: Table 2 shows that among all patients, 73.9% were ≤ 47 years old, 56.7% had a GCS score of ≤ 8, 30.7% had an SBP of ≤ 50 mmHg, and 14.1% had an ISS of ≥ 25. There was no significant difference in early mortality or in-hospital mortality among the different age groups (p=0.99 and p=0.54, respectively). However, significant differences were seen in earlymortality among different GCS scores and SBPs (p=0.001 and p=0.001, respectively) and in in-hospital mortality among different GCS scores, SBPs, and ISSs (p=0.001, p=0.02, and p=0.08, respectively) |
||||||
Table 2: Categorization of clinical factors for early mortality and in-hospital mortality. GCS, Glasgow coma scale; ISS, Injury Severity Score; SBP, systolic blood pressure.
|
Univariate |
Multivariate |
||||||
|
Variables |
|||||||
|
Age |
OR |
95% CI |
OR |
95% CI |
|||
|
< 25 |
Ref |
- |
Ref |
- |
|||
|
25-34 |
1.04 |
0.55-2.00 |
1.04 |
0.47-2.31 |
|||
|
35-46 |
1.01 |
0.51-2.01 |
1.03 |
0.44-2.42 |
|||
|
≥ 47 |
0.95 |
0.49-1.86 |
0.81 |
0.36-1.81 |
|||
|
Gender |
1.41 |
0.81-2.44 |
1.34 |
0.66-2.73 |
|||
|
Male |
|||||||
|
GCS score |
- |
- |
- |
- |
|||
|
14-15 |
Ref |
Ref |
Ref |
Ref |
|||
|
9-13 |
2.77 |
0.63-12.1 |
2.7 |
0.61-12.1 |
|||
|
3-8 |
25.1 |
7.65-82.3 |
25 |
7.50-83.6 |
|||
|
SBP |
- |
- |
- |
- |
|||
|
80-89 |
Ref |
Ref |
Ref |
Ref |
|||
|
71-79 |
1.09 |
0.52-2.27 |
1.23 |
0.54-2.80 |
|||
|
51-70 |
2.03 |
1.07-3.87 |
2.12 |
1.02-4.39 |
|||
|
≤ 50 |
4.15 |
2.01-8.60 |
3.11 |
1.34-7.18 |
|||
|
ISS |
- |
- |
- |
- |
|||
|
< 16 |
Ref |
Ref |
Ref |
Ref |
|||
|
16-24 |
0.81 |
0.37-1.80 |
1.01 |
0.41-2.48 |
|||
|
≥ 25 |
1.22 |
0.60-2.48 |
1.44 |
0.64-3.24
|
|||
|
Note: Table 3 shows the univariate and multivariate logistic regression analysis results for early mortality. A GCS score of ≤ 8 (odds ratio [OR]=25.03, 95% confidence interval [CI]=7.50-83.56) and SBP of ≤ 50.11 mmHg (OR=395% CI=1.34-7.18) were found to be significantly associated with early mortality compared with the reference values (GCS score of 14-15 and SBP of 80-89 mmHg) |
|||||||
Table 3: Univariate and multivariate logistic regression analyses for early mortality OR, odds ratio; CI, confidence interval; GCS, Glasgow coma scale; SBP, systolic blood pressure; ISS, Injury Severity Score; Ref, reference.
|
Univariate |
Multivariate |
|||
|
- |
OR |
95% CI |
OR |
95% CI |
|
Age |
- |
- |
- |
- |
|
<25 |
Ref |
Ref |
Ref |
Ref |
|
25-34 |
0.93 |
0.51-1.71 |
0.72 |
0.32-1.62 |
|
35-46 |
0.89 |
0.47-1.69 |
0.7 |
0.30-1.46 |
|
≥ 47 |
1.36 |
0.73-2.55 |
1.1 |
0.48-2.52 |
|
Gender |
1.06 |
0.63-1.78 |
1.02 |
0.44-1.90 |
|
Male |
||||
|
GCS score |
|
- |
|
- |
|
14-15 |
Ref |
Ref |
Ref |
Ref |
|
Sep-13 |
1.16 |
0.44-3.10 |
1.01 |
0.37-2.79 |
|
03-Aug |
18.9 |
9.28-8.57 |
20.9 |
9.75-44.8 |
|
80- 89 |
Ref |
Ref |
Ref |
Ref |
|
71-79 |
SBP 1.15 |
0.62-2.12 |
1.54 |
0.69-3.43 |
|
51-70 |
1.84 |
1.05-3.25 |
2.19 |
0.90-4.59 |
|
≤ 50 |
2.92 |
1.46-5.83 |
3.16 |
1.05-5.20 |
|
ISS |
- |
- |
|
- |
|
< 16 |
Ref |
Ref |
Ref |
Ref |
|
16-24 |
1.11 |
0,62-1,96 |
1.14 |
0.55-2.39 |
|
≥ 25 |
5.1 |
3.11-8.35 |
2.21 |
1.58-3.10 |
|
Note: Table 4 shows that a GCS score of ≤ 8 (OR = 20.90 and 95% CI=9.75-44.81 compared with the reference GCS score of 14-15), SBP of ≤ 50 mmHg (OR = 3.16 and 95% CI=1.05-5.20 compared with the reference SBP of 80-89 mmHg), and ISS of ≥ 25 (OR=2.21 and 95% CI=1.58-3.10 compared with the reference ISS of < 16) were significantly associated with in-hospital mortality. |
||||
Table 4: Univariate and multivariate logistic regression analyses for in-hospital mortality. OR, odds ratio; CI, confidence interval; GCS, Glasgow coma scale; SBP, systolic blood pressure; ISS, Injury Severity Score; Ref, reference.
Citation: Ton Thanh Tra, Thao T.N Pham, Van Khoi N, Quoc Hung L, Wada K, et al. (2019) Clinical Factors Affecting Mortality in Patients with Traumatic Shock Caused by Road Traffic Accidents Admitted to The Emergency Department: A Prospective Cohort Study. Emerg Med Trauma Care J: EMTCJ-100002.